Disease: Illness or sickness characterized by specific signs and symptoms.
https://web.archive.org/web/20220901051835/https://www.medicinenet.com/disease/definition.htm
Stop me if you've heard this one before. You are in a conversation with someone and the topic of “Covid-19” comes up. You explain that “Covid-19” is nothing more than a new label for the same symptoms of disease that is seen every single year. The idea that there is a new disease was bolstered by a powerful pharmaceutical fear campaign, media hype, and fraudulent PCR testing. There is nothing new under the sun. The other person responds back saying that they know that “Covid-19” is real. They either state that they had “Covid” themselves or that they know someone else who had “it.” They claim that the symptoms were intense and unlike anything that anyone has ever experienced before. Thus, “Covid-19” is a new disease.
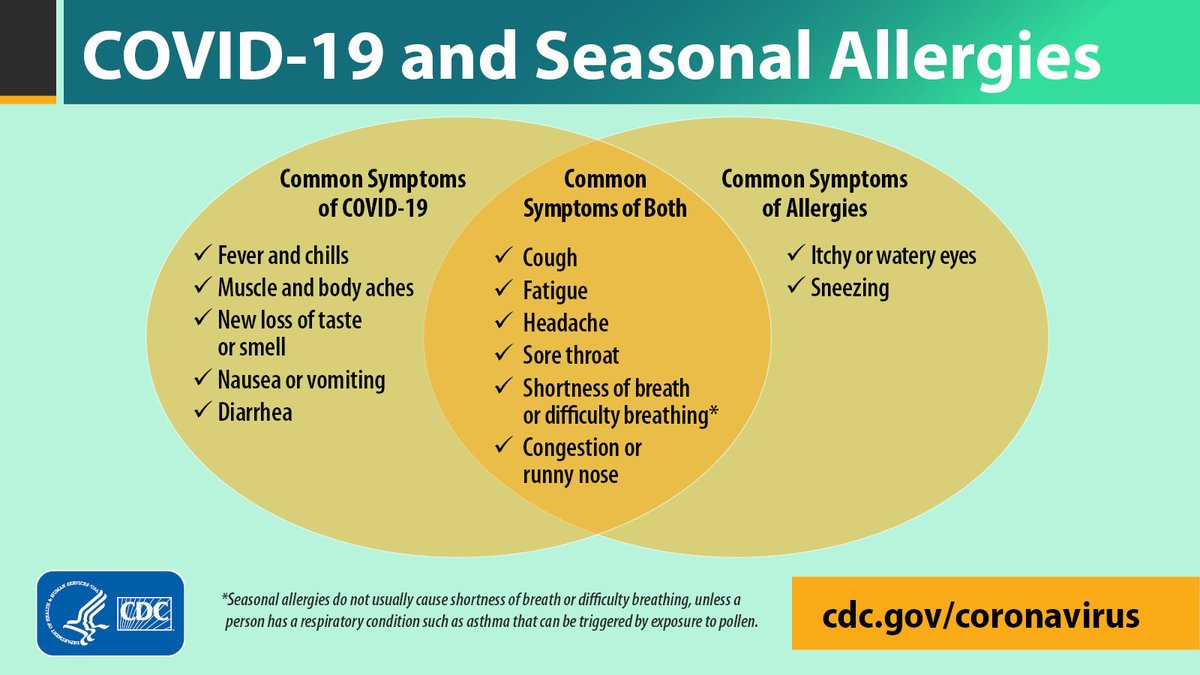
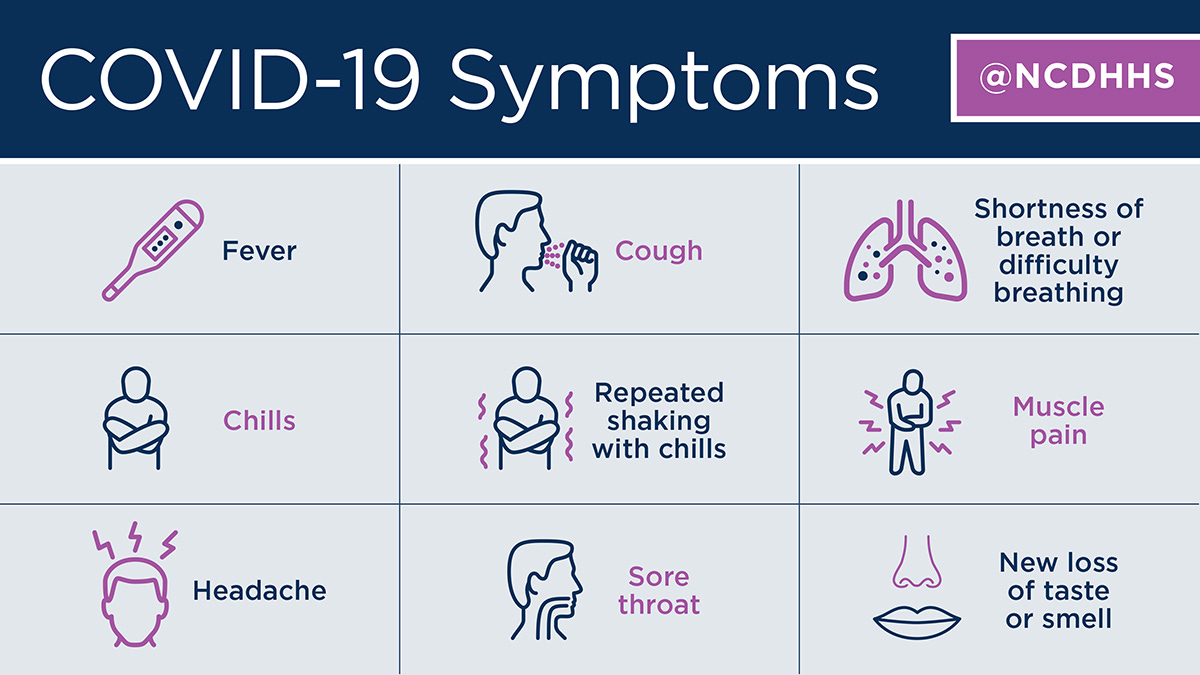
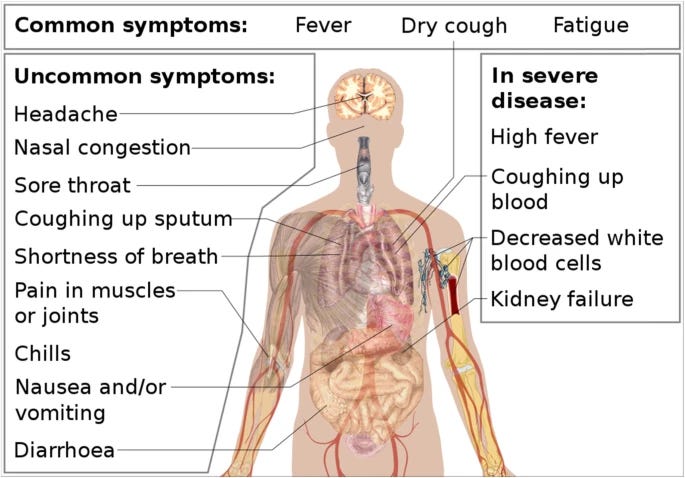
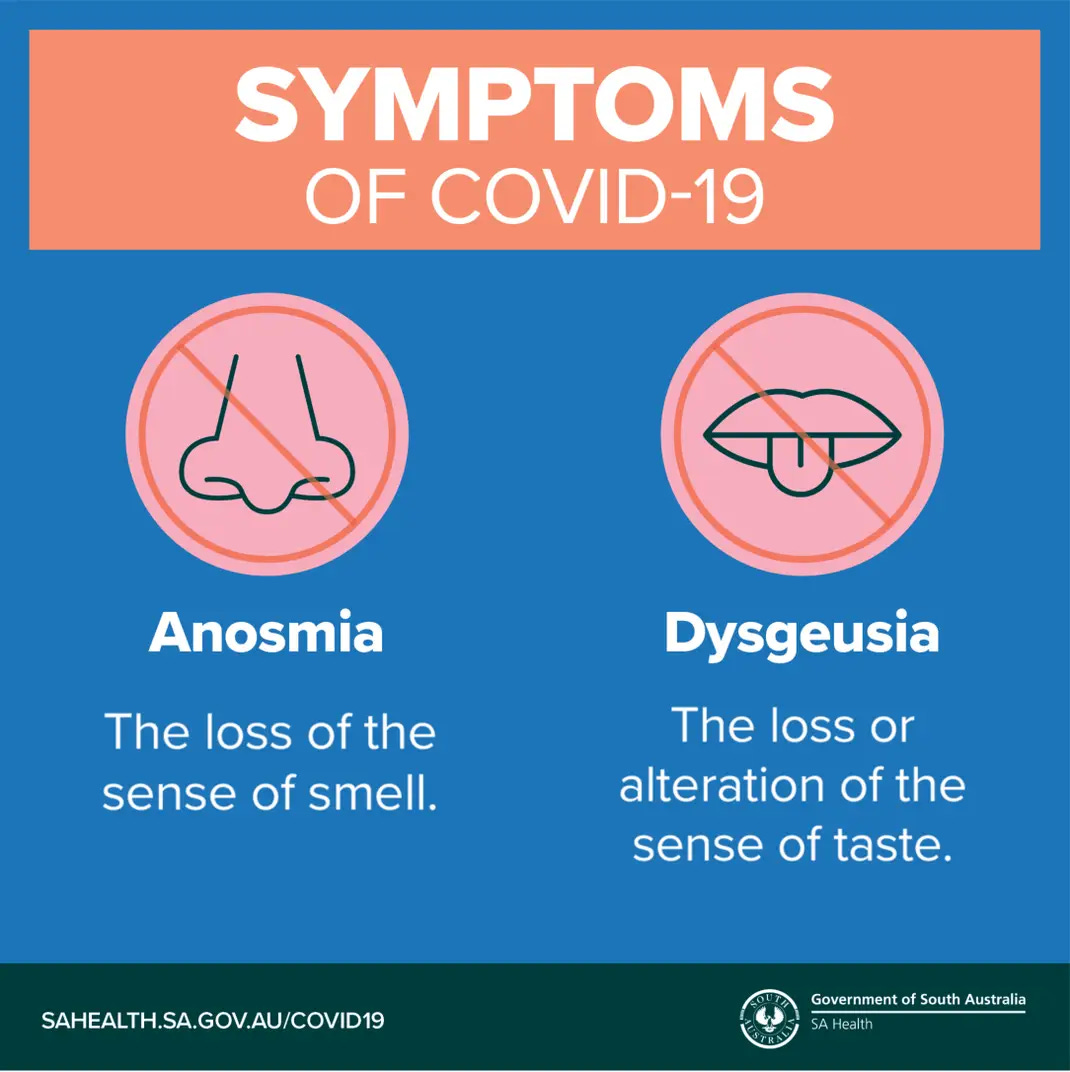
These types of responses are all too common as there is this prevailing belief amongst the population that, in spite of the lack of evidence to support this contention, there are new and specific symptoms that define “Covid-19” as a new disease. For instance, many believe that an acute loss of smell and taste is a new feature that is specific to “Covid.” A media frenzy promoting this as a new sign of the disease became ingrained in the collective consciousness when reports of positive patients experiencing these symptoms began circulating in March 2020. Originally, common indicators such as a fever, cough, and shortness of breath were the main warning signs that we were supposed to look out for if anyone feared that they had “Covid.” However, in late April 2020, the CDC added six more symptoms under the “Covid” umbrella as mass testing began to roll out. These included chills, repeated shaking with chills, muscle pain, headache, sore throat and new loss of taste or smell. In a clever case of subliminal messaging, the word new was often put in front of “loss of taste and smell” as a way to implant the idea that this occurence was previously unheard of.
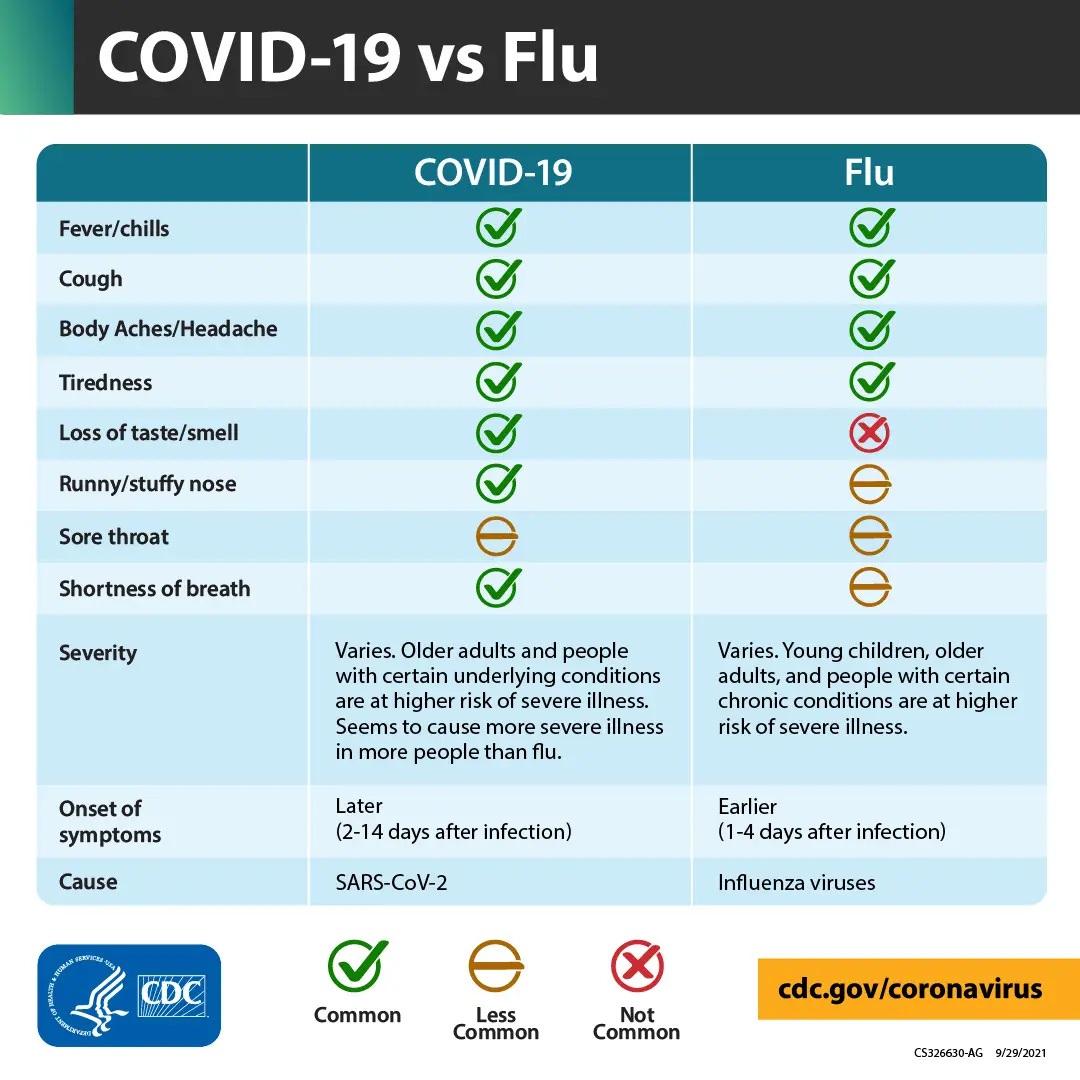
If symptoms were compared between “Covid” and other respiratory diseases, such as the flu, the loss of smell and taste was listed as common to “Covid” with a bright green checkmark, while it was the only symptom listed as uncommon to the flu with a big red X.
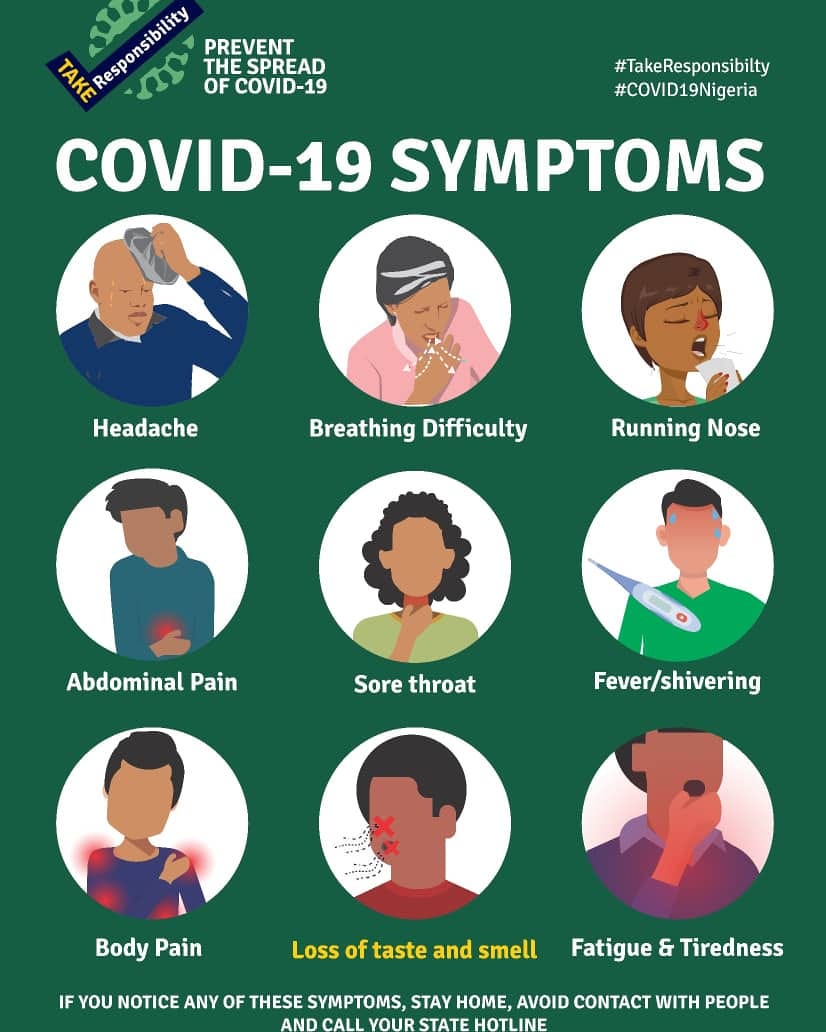
In some very clever subliminal messaging, loss of smell and taste was singled out and highlighted from amongst the other listed symptoms as seen in this propaganda poster from Nigeria.
We were warned that, in many cases, loss of smell and taste were the only symptoms ever experienced by those “infected” who were testing positive for “Covid.”
Stories circulated across the mainstream media stating that the loss of smell and taste were significant and were an early warning sign of “Covid.” Once the CDC listed them amongst the known symptoms, this “confirmed” anecdontal reports from March 2020 that the loss of smell and taste meant that people were otherwise asymptomatic “virus-producing” machines walking around and “infecting” others. In fact, one could be presumed positive for “Covid” based solely upon this phenomenon:
CDC confirms six coronavirus symptoms showing up in patients over and over
“The additions confirm what patients and doctors have been reporting anecdotally for weeks. In particular, the loss of taste or smell has been known to appear in patients since at least mid-March when a British group of ear, nose and throat doctors published a statement amid growing concern that it could be an early sign someone is infected but otherwise asymptomatic.
A study of European covid-19 patients found that between 85.6 percent and 88 percent of patients “reported olfactory and gustatory dysfunctions, respectively.” In an Iranian study, 76 percent of covid-19 patients who reported a loss of smell said it had a sudden onset. In many of the cases, anosmia, as it’s called, appeared before other symptoms.
“It scared the hell out of me,” said Vallery Lomas, a 34-year-old champion baker, who feared she would never get her senses of smell and taste back. “I could smell nothing for probably five days.”
Lomas was presumed positive for covid-19 in the midst of writing a cookbook. Smell and taste are intertwined, so some people who think they have lost both senses may have lost only their sense of smell.”
https://www.washingtonpost.com/health/2020/04/27/six-new-coronavirus-symptoms/
These early reports highlighting lesser known symptoms led people to the belief that there are specific telltale features of a new disease called “Covid-19.” However, is this true, or is it merely media hype? Is the loss of smell and taste really a new and/or specific feature that can identify “Covid” from other respiratory diseases? Are there any other defining signs or symptoms that sets “Covid” apart from the rest of the crowd? Is it even possible for “Covid” to be diagnosed clinically based upon symptoms alone? Are there any laboratory or histopathological findings that distinguishes “Covid” as a new disease? Is “Covid” technically even a “new” disease, or is it simply a rebranding of the same symptoms under a new umbrella term?
What, exactly, is “Covid-19?”
Let's find out.
Defining the Disease
As stated in the introductory quote, a disease is said to be defined by specific signs and symptoms. This definition is backed up by various sources as seen here, here, and here. In order to answer the question as to whether there are any new and/or specific signs or symptoms related to “Covid” that allow the disease to be easily defined as something new, we must start at the beginning. The world was first alerted to the presence of a pneumonia of unknown cause coming from China by the WHO on January 5th, 2020. In the statement, the WHO admitted that no causative agent had been identified, and that the symptoms experienced in these cases were common, especially during the winter months. In other words, the only reason for the alert was that no cause through testing could be associated with these cases of typical pneumonia:
Pneumonia of unknown cause – China
“On 31 December 2019, the WHO China Country Office was informed of cases of pneumonia of unknown etiology (unknown cause) detected in Wuhan City, Hubei Province of China. As of 3 January 2020, a total of 44 patients with pneumonia of unknown etiology have been reported to WHO by the national authorities in China. Of the 44 cases reported, 11 are severely ill, while the remaining 33 patients are in stable condition. According to media reports, the concerned market in Wuhan was closed on 1 January 2020 for environmental sanitation and disinfection.
The causal agent has not yet been identified or confirmed. On 1 January 2020, WHO requested further information from national authorities to assess the risk.”
“There is limited information to determine the overall risk of this reported cluster of pneumonia of unknown etiology. The reported link to a wholesale fish and live animal market could indicate an exposure link to animals. The symptoms reported among the patients are common to several respiratory diseases, and pneumonia is common in the winter season; however, the occurrence of 44 cases of pneumonia requiring hospitalization clustered in space and time should be handled prudently.”
https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229
Turning to the initial studies from China, we can glean some more information as to what these common symptoms were that necessitated an alert by the WHO. According to the Fan Wu et al. paper that provided the genome of the compuer-generated “virus” that was eventually blamed as the cause, the 41-year-old patient the genome was obtained from suffered the non-specific symptoms of fever, dizziness, and a cough:
A new coronavirus associated with human respiratory disease in China
“Here we study a single patient who was a worker at the market and who was admitted to the Central Hospital of Wuhan on 26 December 2019 while experiencing a severe respiratory syndrome that included fever, dizziness and a cough.”
“The patient studied was a 41-year-old man with no history of hepatitis, tuberculosis or diabetes. He was admitted to and hospitalized in the Central Hospital of Wuhan on 26 December 2019, 6 days after the onset of disease. The patient reported fever, chest tightness, unproductive cough, pain and weakness for 1 week on presentation (Table 1).”
https://www.nature.com/articles/s41586-020-2008-3
A companion study by Zhou et al. stated that the main symptoms experienced by the initial patients were fever, headache, dry cough, difficulty breathing, and pneumonia:
A pneumonia outbreak associated with a new coronavirus of probable bat origin
“Here we report on a series of cases caused by an unidentified pneumonia disease outbreak in Wuhan, Hubei province, central China. This disease outbreak—which started from a local seafood market—has grown substantially to infect 2,761 people in China, is associated with 80 deaths and has led to the infection of 33 people in 10 additional countries as of 26 January 202012. Typical clinical symptoms of these patients are fever, dry cough, breathing difficulties (dyspnoea), headache and pneumonia.”
https://www.nature.com/articles/s41586-020-2012-7
A related study by Zhu et al. examined three early patients presenting with pneumonia of an unknown cause. Symptoms were only available for two of the patients, and these included fever, cough, and chest discomfort:
A Novel Coronavirus from Patients with Pneumonia in China, 2019
“Three adult patients presented with severe pneumonia and were admitted to a hospital in Wuhan on December 27, 2019. Patient 1 was a 49-year-old woman, Patient 2 was a 61-year-old man, and Patient 3 was a 32-year-old man. Clinical profiles were available for Patients 1 and 2. Patient 1 reported having no underlying chronic medical conditions but reported fever (temperature, 37°C to 38°C) and cough with chest discomfort on December 23, 2019. Four days after the onset of illness, her cough and chest discomfort worsened, but the fever was reduced; a diagnosis of pneumonia was based on computed tomographic (CT) scan. Her occupation was retailer in the seafood wholesale market. Patient 2 initially reported fever and cough on December 20, 2019; respiratory distress developed 7 days after the onset of illness and worsened over the next 2 days (see chest radiographs, Figure 1), at which time mechanical ventilation was started. He had been a frequent visitor to the seafood wholesale market.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092803/
Thus, we can clearly see that there was nothing unusual about the symptoms experienced at the time “Covid” began to make the headlines. The disease that all of the patients were said to be suffering from was a pneumonia of an “unknown cause” presenting with common symptoms such as fever, cough, headache, dizziness, and difficulty breathing. There were absolutely no distinguishing signs or symptoms differentiating a “Covid” case from anyone suffering these same symptoms of disease other than the presumed “novel” cause.
Perhaps understanding that there was a need for a defining symptom, the often-ignored loss of smell and taste emerged early on as a leading sign that one was suffering from “Covid.” A March 2020 article by the New York Times presented anosmia (loss of smell) and ageusia (loss of taste), two symptoms that typically go hand-in-hand together, to the world as peculiar signs of the disease. Doctors were calling on anyone who experienced these symptoms to isolate in order to stop the “spread” of the “virus,” even if they had no other accompanying symptoms. The doctors wanted to raise awareness that losing one's sense of smell and taste was a sign of “infection.” They urged all healthcare workers who examined patients experiencing these symptoms to wear protective gear, and recommended against doing any sinus endoscopy procedures over fear that this may release “virus” and expose workers. Evidence was cited that 30 percent of the patients testing positive were suffering from anosmia as their major presenting symptom. The American Academy of Otolaryngology stated that losing taste and smell were significant symptoms of “Covid-19.” Doctors in Italy concluded that, even if a person appeared healthy, anyone experiencing these symptoms were carrying the “virus” and “infecting” others:
Lost Sense of Smell May Be Peculiar Clue to Coronavirus Infection
Doctor groups are recommending testing and isolation for people who lose their ability to smell and taste, even if they have no other symptoms.
“A mother who was infected with the coronavirus couldn’t smell her baby’s full diaper. Cooks who can usually name every spice in a restaurant dish can’t smell curry or garlic, and food tastes bland. Others say they can’t pick up the sweet scent of shampoo or the foul odor of kitty litter.
Anosmia, the loss of sense of smell, and ageusia, an accompanying diminished sense of taste, have emerged as peculiar telltale signs of Covid-19, the disease caused by the coronavirus, and possible markers of infection.
On Friday, British ear, nose and throat doctors, citing reports from colleagues around the world, called on adults who lose their senses of smell to isolate themselves for seven days, even if they have no other symptoms, to slow the disease’s spread. The published data is limited, but doctors are concerned enough to raise warnings.
“We really want to raise awareness that this is a sign of infection and that anyone who develops loss of sense of smell should self-isolate,” Prof. Claire Hopkins, president of the British Rhinological Society, wrote in an email. “It could contribute to slowing transmission and save lives.
She and Nirmal Kumar, president of ENT UK, a group representing ear, nose and throat doctors in Britain, issued a joint statement urging health care workers to use personal protective equipment when treating any patients who have lost their senses of smell, and advised against performing nonessential sinus endoscopy procedures on anyone, because the virus replicates in the nose and the throat and an exam can prompt coughs or sneezes that expose the doctor to a high level of virus.”
“The British physicians cited reports from other countries indicating that significant numbers of coronavirus patients experienced anosmia, saying that in South Korea, where testing has been widespread, 30 percent of 2,000 patients who tested positive experienced anosmia as their major presenting symptom (these were mild cases).
The American Academy of Otolaryngology on Sunday posted information on its website saying that mounting anecdotal evidence indicates that lost or reduced sense of smell and loss of taste are significant symptoms associated with Covid-19, and that they have been seen in patients who ultimately tested positive with no other symptoms.”
“In the areas of Italy most heavily affected by the virus, doctors say they have concluded that loss of taste and smell is an indication that a person who otherwise seems healthy is in fact carrying the virus and may be spreading it to others.
“Almost everybody who is hospitalized has this same story,” said Dr. Marco Metra, chief of the cardiology department at the main hospital in Brescia, where 700 of 1,200 inpatients have the coronavirus. “You ask about the patient’s wife or husband. And the patient says, ‘My wife has just lost her smell and taste but otherwise she is well.’ So she is likely infected, and she is spreading it with a very mild form.”
However, for anyone doing a cursory bit of research outside of the mainstream propaganda, it was abundantly clear that the loss of smell and taste were not new symptoms of disease nor were they specific to “Covid-19.” These symptoms are often associated with allergies, the common cold, influenza, drug reactions, head injuries, old age, etc. In an April 2020 interview with experts in anosmia, VCU School of Medicine faculty Richard Costanzo, Ph.D. and Evan Reiter, M.D., it is said that many people experience these symptoms without ever noticing that they are present until someone alerts them to it. Both men stated that it is a common occurrence and that there are many potential causes:
Are there other potential causes of loss of smell?
Costanzo: If people think that, “Oh, if you lose your sense of smell, it means you have COVID-19,” there are a lot of people that will notice, if you bring to their attention, that their sense of smell is not that good. Especially in the elderly, it’s a common occurrence as people get older and there are other conditions that can cause a loss of smell. So to call it a predictor of COVID-19 is premature.
Reiter: Yes. Given that there are a lot of people who are presumed positive but are not being tested, there are other respiratory viruses still around, including flu itself. And some of these other viruses, including rhinoviruses — which are commonly implicated in the common cold — other coronaviruses and influenza, also have been implicated in causing a loss of sense of smell.
https://www.vcuhealth.org/news/covid-19/what-does-loss-of-smell-mean-during-covid-19
While still highlighting loss of smell and taste as a potential sign of a “Covid infection,” an article from PositiveMed.com also pointed out that this is not a specific, nor a uniquely distinctive feature of "Covid,” and that it is actually quite common in respiratory disease:
Lost Sense Of Smell May Be Peculiar Clue To Coronavirus Infection
“The American Academy of Otolaryngology-Head and Neck Surgery believe that detecting anosmia and dysgeusia can indicate the COVID-19 infection. Anosmia is the total or partial loss of the sense of smell, while ageusia is the loss of taste functions of the tongue. These symptoms are now officially added to the list of screening tools for the illness. However, a diminished sense of taste and smell can be symptomatic of a wide variety of illnesses, respiratory or otherwise. It’s not a specific, nor a uniquely distinctive feature of COVID-19. A temporary loss or reduction in your smell or taste during every respiratory infection is quite common.”
Thus, it is clear that, contrary to popular belief, losing one's sense of smell and taste is not unique to “Covid,” even though the media highlighted this as a defining characteristic of “Covid.” They began a campaign to alert the public to be on the lookout for such a problem in order to be tested in the instance it occurs. Because of this increased awareness, rather than ignoring any smell and taste abnormalities as was the case prior to “Covid,” this common occurrence became the rallying cry for the emergence of a new disease. However, the loss of smell and taste is clearly not specific to “Covid,” and one cannot use it in order to claim that “Covid” is a new disease.
As the main symptoms associated with “Covid” are common amongst many different diseases that are attributed to many different causes, there is no realistic way to clinically diagnose someone with “Covid” based upon symptoms alone. This inability to distinguish a “Covid” patient from someone with respiratory disease attributed to another cause based upon clinical symptoms is a well-known fact:
The newly emerged COVID-19 disease: a systemic review
"Even though COVID-19 manifest with different symptoms, none of these symptoms are present in every patient and there are no specific signs or symptoms that could suggest COVID-19 compared to symptoms and signs of respiratory illnesses caused by other viruses, such as influenza and common cold [21, 23].”
https://virologyj.biomedcentral.com/articles/10.1186/s12985-020-01363-5
Diagnosing COVID-19: The Disease and Tools for Detection
“The symptoms expressed by COVID-19 patients are nonspecific and cannot be used for an accurate diagnosis. Guan et al. reported that 44% of 1099 COVID-19 patients from China had a fever when they entered the hospital and that 89% developed a fever while in hospital.25 They further found that patients had a cough (68%), fatigue (38%), sputum production (34%), and shortness of breath (19%). Many of these symptoms could be associated with other respiratory infections.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7144809/
The lack of specificity and an inability to diagnose a “Covid” case clinically is supported by the British Medical Journal (BMJ) Best Practice Guidelines which states:
“No single sign or symptom can accurately diagnose COVID-19, and neither the absence or presence of specific signs or symptoms are accurate enough to rule in or rule out disease.”
This was backed up as well by a September 2021 study that attempted to create a differential diagnosis between “Covid” and other diseases. The authors concluded that “Covid” cannot be differentiated from other respiratory infections via clinical signs, symptoms, or laboratory results. The symptoms defining “Covid” are non-specific and overlapped with many other conditions. The researchers admitted that establishing differential diagnosis criteria remained very challenging and that clinical discrimination was unreliable as there were no clinical or laboratory parameters that could be relied upon:
What about the others: differential diagnosis of COVID-19 in a German emergency department
“For many common ED diagnoses, COVID-19 should be considered a differential diagnosis. COVID-19 cannot be distinguished from COVID-19 negative respiratory infections by clinical signs, symptoms, or laboratory results. When hospitalization is necessary, the clinical course of COVID-19 airway infections seems to be more severe compared to other respiratory infections.”
Discussion
“Early triage and differential diagnosis of patients presenting with typical clinical symptoms of COVID-19 remain very challenging but relevant. Our study had the following main findings:
Differential diagnosis of typical COVID-19 symptoms is very broad and comprises many common respiratory, infectious, and cardiovascular diseases, whereas respiratory diseases are the most frequent. Diseases from nearly every field of clinical medicine can mimic a clinical picture like that of COVID-19, with respiratory diseases being the most prevalent. Older patients may be even more challenging since the clinical picture may be atypical with syncope and malaise [12].
Patients with COVID-19 present with similar symptoms as COVID-19 negative respiratory infections, so clinical discrimination is not reliable.”
Conclusions
“Differential diagnoses of COVID-19 are plentiful and comprise many common diseases, most notably ailments associated with respiratory impairment. Triage remains challenging in the emergency department since there are no reliable clinical or laboratory parameters to distinguish safely between COVID-19 and airway infections of other origins. When inpatient, COVID-19 takes a more severe clinical course than comparable COVID-19 negative airway infections. Therefore, a strict isolation policy together with broad and rapid testing will remain the most important measures for the months to come.”
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06663-x
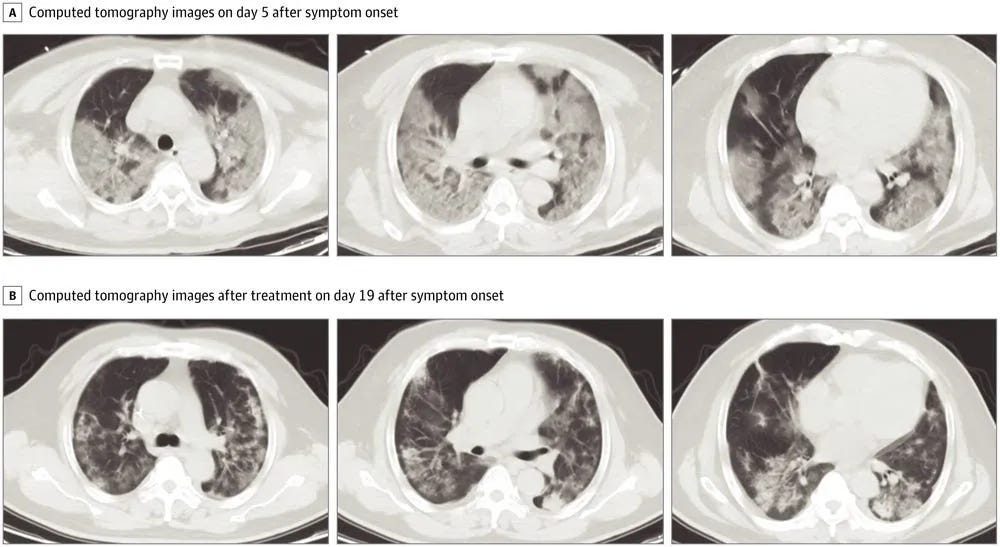
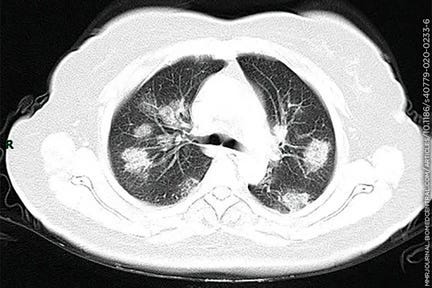
As there was a failure to present any unique and defining symptoms for “Covid,” and there was an inability to distinguish the “new” disease from others based upon symptoms alone, there needed to be some other sign that helped “Covid” to stand out from amongst the crowd. There were early attempts to make the case that certain histopathological findings, such as chest x-rays revealing ground-glass opacities, were a way to distinguish “Covid” patients from any others presenting with the same symptoms. This finding became one of the early defining characteristics that was used to diagnose a “Covid” case. An April 2020 article by the New York Times helped to drum up fear over this particular phenomenon by stating that “Covid” patients with an “insidious pneumonia” have this hazy appearance in the lower regions of the lungs on CT scans:
Why Days 5 to 10 Are So Important When You Have Coronavirus
“But tracking symptoms and paying special attention as the illness nears its second week has taken on new urgency as more doctors are seeing patients arriving at the hospital with an insidious form of pneumonia. On scans, patients with Covid pneumonia have a finding called “ground-glass opacities,” a hazy appearance in the lower part of both lungs. Oxygen levels may drop so slowly that the patient doesn’t even notice, a condition called silent hypoxia. Often it is not until oxygen saturation reaches dangerously low levels, causing severe shortness of breath, that they finally seek care.”
A June 2020 article in Vox stated that the lungs of “Covid” patients are affected by lighter gray patches when compared to healthy lungs. The article shared evidence from China stating that 77% of the “Covid” patients had this feature. In another Chinese study, 66 of 70 patients presented with this type of lung damage. However, these same images were seen in 95% of the asymptomatic, i.e. healthy cases, as well:
The emerging long-term complications of Covid-19, explained
“It is a true roller coaster of symptoms and severities, with each new day offering many unknowns.”
“On CT scans, while normal lungs appear black, Covid-19 patients’ lungs frequently have lighter gray patches, called “ground-glass opacities” — which may not heal.
One study from China found that this ground-glass appearance showed up in scans of 77 percent of Covid-19 patients. In another study out of China, published in Radiology, 66 of 70 hospitalized patients had some amount of lung damage in CT scans, and more than half had the kind of lesions that are likely to develop into scars. (A third study from China suggests this is not just for critically ill patients; its authors found that of 58 asymptomatic patients, 95 percent also had evidence of these ground-glass opacities in their lungs. More than a quarter of these individuals went on to develop symptoms within a few days.)”
The CDC also pointed out that multiple studies have suggested that these abnormalities on CT or chest radiograph “may be present in people who are asymptomatic, pre-symptomatic, or before RT-PCR detection of SARS-CoV-2 RNA in nasopharyngeal samples.” In other words, the ground-glass opacities are found in people free of disease and without a positive “Covid” PCR test. However, that didn't stop the media from attempting to highlight this ground-glass opacity phenomenon as a key feature of “Covid,” even though it is actually found in many conditions, including in those who vape:
Many coronavirus patients have 'ground glass' in their lung scans. Here's what that looks like.
“Patients with severe cases typically develop fluid in their lungs, similar to those seen in standard pneumonia cases. That fluid can be detected on a CT scan, where it shows up in the form of white patches that doctors call "ground glass."
CT scans are considered less thorough than lab tests, but here's what physicians look for to detect the coronavirus in a scan.”
“On its own, Lakhani said, ground glass isn't particularly helpful for identifying a coronavirus.
"You can see it with all types of infections — bacterial, viral, or sometimes even non-infectious causes," Lakhani said. "Even vaping could sometimes appear this way."
Despite the media highlighting this ground-glass opacity phenomenon, it was known that using CT scans as a method of detection was non-specific and that it did not even match up with PCR results. In other words, there were cases of those who had the ground glass opacities while testing negative via PCR and those who did not have the finding and still tested positive for “Covid” via PCR. In some cases where there was no suspicion of “Covid,” people were imaged for other health problems and ended up being diagnosed as a “Covid” patient due solely to the unrelated finding of non-specific ground-glass opacities:
Hazy on Ground-Glass Opacities? Here's What They Are
— Frequent finding in COVID-19, but how disease-specific is it?
“Essentially, a ground-glass opacity describes the "shades of greyopens in a new tab or window" in between a normal lung scan and one from an extremely diseased lung that shows up nearly all white because it's full of puss or fluid, said Henry Guo, MD, PhD, of Stanford University in Palo Alto, California.”
"We see [ground-glass opacities] so often in chest imaging," Guo told MedPage Today. They come in different shapes, sizes, quantities, and locations, and they can indicate many different underlying pathologies -- including other viral infections, chronic lung disease, fibrosis, other inflammatory conditions, and cancers.”.
“They also had many cases where COVID-19 wasn't initially suspected but was detected incidentally. For instance, patients who had gastrointestinal issues but no respiratory symptoms were sent for abdominal CT, which catches the bottom of the lungs. "In many cases we saw ground-glass opacities" and those patients were subsequently diagnosed with COVID-19, he said.
Matthew Cham, MD, of the University of Washington in Seattle, said there was initial hope as one study determined that CT can show ground-glass opacities during the first few days of COVID infection, when PCR testing may be especially susceptible to false negatives.
"This initial observation led to substantial excitement around the potential usefulness of chest CTs for the early detection of COVID-19," Cham told MedPage Today.
Subsequent studies, however, showed some COVID patients have normal chest CTs with no ground-glass opacities during the first few days of the infection, Cham said.”
https://www.medpagetoday.com/pulmonology/generalpulmonary/86751
It is known that the accuracy of a CT scan finding depends upon community prevalence of a disease, which is a factor that also affects the claimed accuracy of PCR results. When disease prevalence is low, false positives are high. However, in order to determine disease prevalence, the disease must be able to be diagnosed clinically so that cases can be calculated. As we've already seen, due to a lack of specific signs and symptoms of disease, “Covid” cannot be diagnosed clinically. Thus, just as in the case with PCR, there is no way to determine an accurate disease prevalence rate in order to establish the accuracy of the CT scans:
Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era
“The purpose of this review is to discuss and differentiate typical imaging findings of COVID-19 from those of other diseases, which can appear similar in the first instance. The typical CT findings of COVID-19 are bilateral and peripheral predominant ground-glass opacities. As per the Fleischner Society consensus statement, CT is appropriate in certain scenarios, including for patients who are at risk for and/or develop clinical worsening. The probability that CT findings represent COVID-19, however, depends largely on the pretest probability of infection, which is in turn defined by community prevalence of infection. When the community prevalence of COVID-19 is low, a large gap exists between positive predictive values of chest CT versus those of reverse transcriptase polymerase chain reaction. This implies that with use of chest CT there are a large number of false-positive results. Imaging differentiation is important for management and isolation purposes and for appropriate disposition of patients with false-positive CT findings.”
https://pubs.rsna.org/doi/full/10.1148/radiol.2020202504
Beyond the inability to diagnose “Covid” based upon CT scans and the non-specific ground-glass opacity phenomenon, it is said that other histopathologic findings are non-specific as well. In an August 2020 review on the pathological picture of “Covid,” the researchers stated that the overall pathologic findings are similar to those reported in “H1N1” (swine flu) and “SARS1.” The gross macroscopic findings in “Covid” patients are non-specific. Autopsies showed non-specific histopathologic findings, none of which are pathognomonic of “Covid.” Diffuse alveolar damage (DAD) in “Covid” patients could not be differentiated from the other etiologies of DAD by morphologic evaluation. It was noted that there is no consistent or pathognomonic “viral” cytopathic effects. The authors stated that the pathology described in organs is far from specific, and it is unclear whether the changes described reflected “viral” infection or underlying/pre-existing conditions. Even cardiac findings were non-specific, and there was no evidence that myocarditis was a common occurrence in “Covid” patients:
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19) – anatomic pathology perspective on current knowledge
Pathologic features of COVID-19
“There is currently a paucity of pathologic data on COVID-19, most of it being derived from observations reported in a few post-mortem biopsies, two lung cancer lobectomies, a handful of limited autopsies and only a few complete autopsies, including 2 recent series [27, 38,39,40,41,42,43,44,45,46,47,48]. Published reports are summarized in Table 2. Although autopsy data are limited, overall the pathologic findings reported thus far are similar to those reported in H1N1 (swine flu) [60] and SARS [61].
Macroscopic features
Gross findings in COVID-19 are non-specific. The lungs are heavy, with bilateral interstitial edema and congestion [39, 41, 44]. The cut surfaces show tan-grey consolidation and/or patchy hemorrhagic areas [27].”
Microscopic features
“Autopsy data have thus far revealed non-specific histopathologic findings, none of which are pathognomonic of COVID-19; pulmonary changes have been the most noteworthy.”
“These changes are frequently encountered in other infectious and non-infectious causes of DAD [60,61,62]. No consistent or pathognomonic viral cytopathic effects have yet been established [38, 41]. One study reported remarkable capillary congestion observable in all 21 specimens, irrespective of DAD, accompanying suppurative pneumonia etc. [27].”
“The pathology described in other organs is far from specific, and it is unclear whether the changes described reflect viral infection or underlying/pre-existing conditions.”
“Cardiac findings reported thus far have been non-specific and focal [27, 47]. They include “scattered individual myocyte necrosis and scattered lymphocytic infiltrate” in one case [69] and “lymphocytic myocarditis” in the right ventricle in another [47]. There is no pathologic evidence thus far that myocarditis is a common occurrence in COVID-19.”
https://diagnosticpathology.biomedcentral.com/articles/10.1186/s13000-020-01017-8
This fact that the pathological picture of “Covid” is non-specific was backed up by an August 2022 review which stated that “the respiratory distress and the gross pathological changes observed in COVID-19 are not specific.” Thus, there is no way to determine a “Covid” patient from a non-"Covid” patient by examining the tissues, organs, and cells of those claimed to be suffering from a new disease. Unsurprisingly, this inability to define “Covid” based upon clinical, laboratory, and histopathological methods did not stop the WHO from naming the exact same symptoms of disease with a new label.
According to Science, “Covid-19” became the name for the new disease “paralyzing China and threatening the rest of the world” on February 11th, 2020. Coincidentally, or not, at the exact moment WHO head Tedros Adhanom Ghebreyesus named the “new disease,” the Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses decided that the “virus” should be called “SARS-COV-2” based upon its not-so-significant genomic relationship to “SARS-COV-1.” Thus, the stage was set for a “new disease” with a “new cause,” even though neither actually existed. Ironically, Mike Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, stated that he would not use the name “SARS-COV-2” as “SARS” was a “different disease” from “Covid:”
Update: ‘A bit chaotic.' Christening of new coronavirus and its disease name create confusion
"COVID-19. I'll spell it: C-O-V-I-D hyphen one nine. COVID-19."
That's how Tedros Adhanom Ghebreyesus, head of the World Health Organization (WHO), introduced the agency's official name for the new disease that's paralyzing China and threatening the rest of the world. The christening yesterday, at one of WHO's now daily outbreak press conferences in Geneva, ended 6 weeks of uncertainty about what the disease would be called—but it also created some new confusion.
COVID-19 is a name for the disease, not for the virus that causes it, which until now had a temporary moniker, 2019-nCoV, signifying it was a novel coronavirus that emerged last year. But the pathogen also got a new designation, which arrived before Tedros had even finished his press conference, by way of a preprint posted on bioRxiv by the body charged with classifying and naming viruses. The Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses, the paper noted, had decided that the virus is a variant of the coronavirus that caused an outbreak of severe acute respiratory syndrome (SARS) in 2002–03. So, it named the new pathogen severe acute respiratory syndrome-related coronavirus 2, or SARS-CoV-2.”
“Mike Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, says he won't use the name SARS-CoV-2 either. "We don't believe it is an accurate name, actually confusing a quite different disease (SARS) with this one (COVID-19)," Osterholm says.”
What is “Covid-19?”
We know that there are no characteristic signs and symptoms that define “Covid” as a new disease. We know that there are no clinical, laboratory, and histopathological parameters that can be used to identify “Covid” as a new disease. So what exactly is “Covid-19?” Let's see what the “experts” say.
According to the CDC, “Covid” is simply a disease caused by “SARS-COV-2” that can feel like the common cold, flu, or pneumonia:
“COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2.”
“COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia.”
https://www.cdc.gov/coronavirus/2019-ncov/your-health/about-covid-19.html
According to the WHO, “Covid” is an “infectious” disease that is caused by “SARS-COV-2” which results in mild to moderate respiratory illness:
“Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus.
Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment.”
https://www.who.int/health-topics/coronavirus#tab=tab_1
According to the European CDC, “Covid” is a respiratory disease sharing symptoms with the flu, with the only difference separating the two illnesses being the scientifically unproven “viral” cause:
“Coronavirus disease 2019 (COVID-19) is the respiratory disease caused by SARS-CoV-2.”
“Influenza, also known as the flu, is a respiratory illness that has similar symptoms but is caused by influenza viruses, not coronaviruses.”
https://www.ecdc.europa.eu/en/covid-19/questions-answers/questions-answers-basic-facts
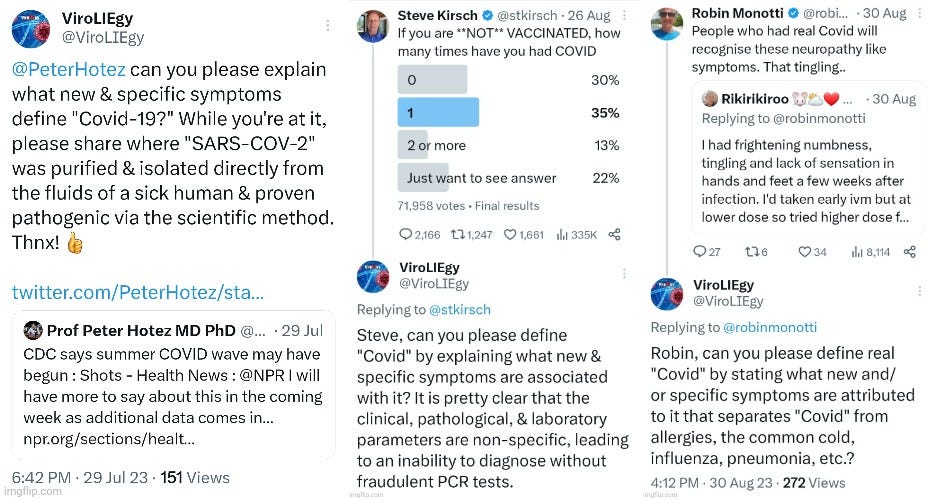
Thus, we can see that the common denominator in all definitions is that “Covid-19” is simply the same symptoms of respiratory disease regularly experienced as the common cold, influenza, and pneumonia with the only defining difference between them being the scientifically unproven causative agent. There is no new disease. There is only a new “cause.” Knowing this, I've asked many people who defend germ theory and virology, and even those who are within the “health freedom movement” who promote the same lies, to please define “Covid-19” for me. I want them to explain how “Covid-19” is any different from diseases past, beyond the scientifically unproven “viral” cause. I have found that, more often than not, I get nothing but crickets, as seen when I asked this question of Peter Hotez, Steve Kirsh, and Robin Monotti.
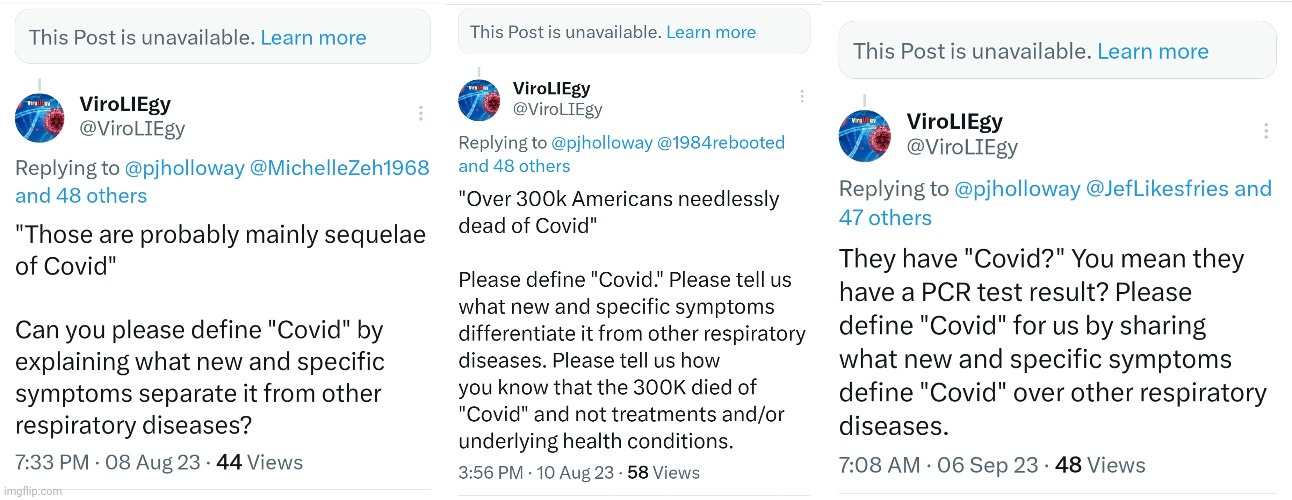
Other times, not only do I get crickets, but the tweets that I had responded to challenging an individual to define “Covid” are either deleted or unavailable for some strange reason.
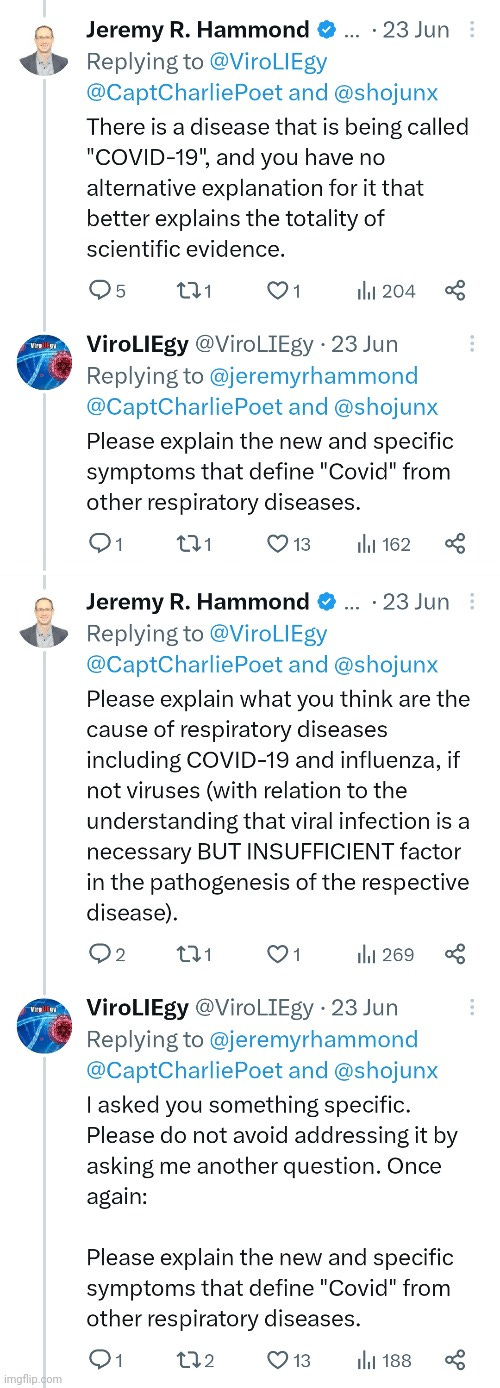
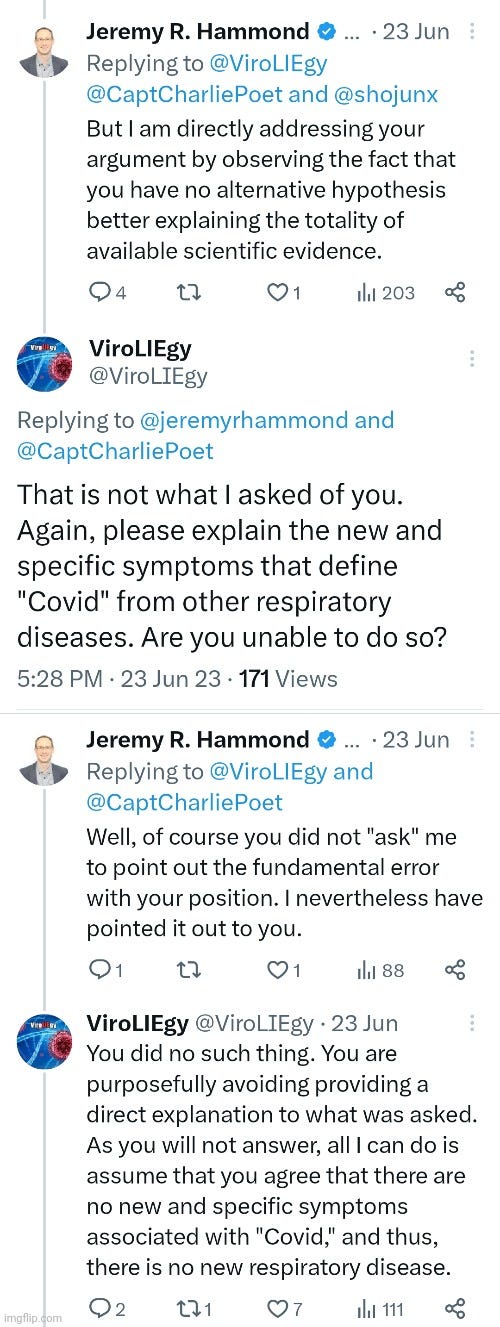
However, every so often, someone will try to dance around providing a direct answer as to what “Covid-19” is, as was seen with Jeremy Hammond recently. Rather than answer me directly, Jeremy attempted to logically fallaciously shift away from his burden of defining “Covid” by telling me to provide an alternative explanation for the cause of the disease.
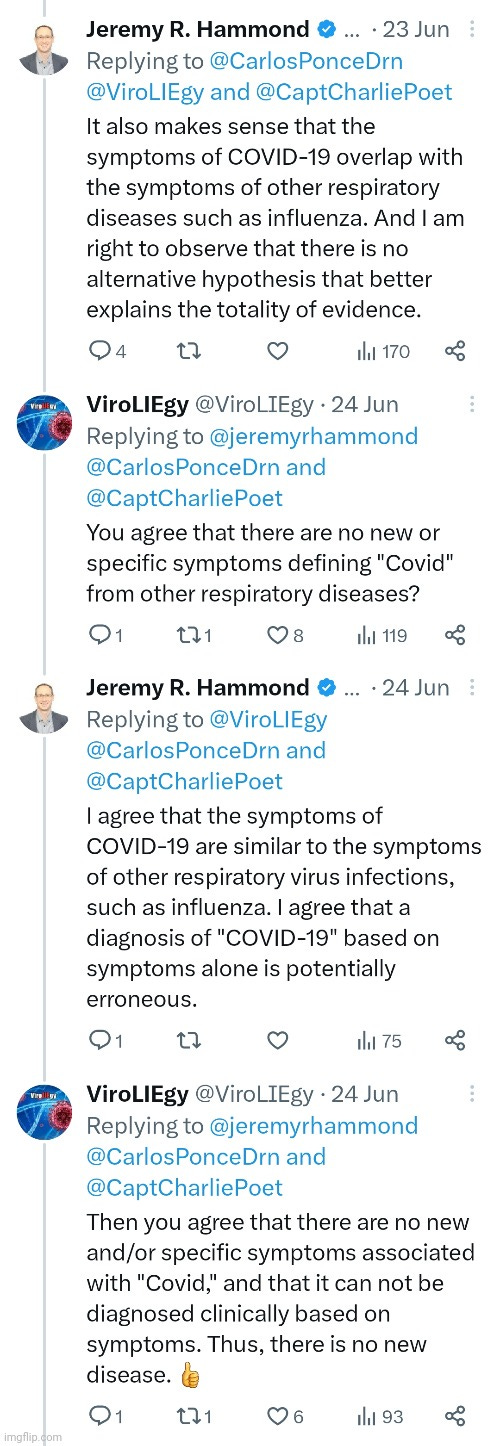
In response to another user @CarlosPonceDrn, Jeremy stated that the symptoms of “Covid” overlapped with other respiratory diseases, thus admitting that there were no new and/or specific symptoms defining it. He admitted to me in my follow-up that clinical diagnosis based solely upon symptoms is erroneous.
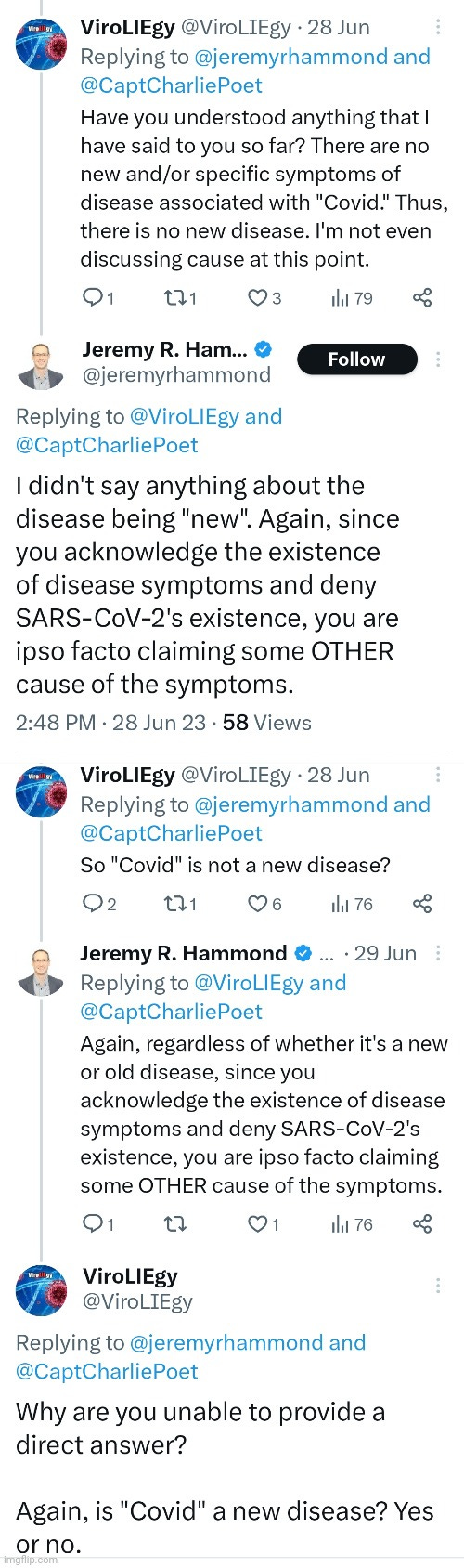
In an exchange a few days later, Jeremy stated that he never said “Covid” was a new disease. Thus, his only argument was that there was a new cause of the same symptoms of disease. While it was clear that Jeremy knows full well that “Covid” is not a new disease, I wanted him to provide a direct answer to my question. When I tried to get Jeremy to provide a direct YES or NO as to whether or not “Covid” was a new disease, he went silent.
When we break down what “Covid-19” truly is, it is no wonder why so many people have trouble defining and explaining how “Covid” is a new disease. There is absolutely no evidence that a new disease exists. What we have is a new label for the same symptoms seen every single year that are regularly presented under various other labels. “Covid-19” is simply the latest name to enter the ring. As there are no defining signs and symptoms and there is no way to identify “Covid” based upon clinical, laboratory, or histopathological methods, it falls upon the fraudulent PCR tests to diagnose a “Covid” case. This was admitted by the CDC when they stated that illnesses such as the flu and “Covid” cannot be differentiated via symptoms alone, thus requiring PCR tests for diagnosis:
“You cannot tell the difference between flu and COVID-19 by symptoms alone because some of the symptoms are the same. Some PCR tests can differentiate between flu and COVID-19 at the same time. If one of these tests is not available, many testing locations provide flu and COVID-19 tests separately.”
https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
However, PCR was never meant to diagnose disease as anyone can test positive for practically anything using this method, and it is unable tell you that you’re sick as described by PCR inventor Kary Mullis:
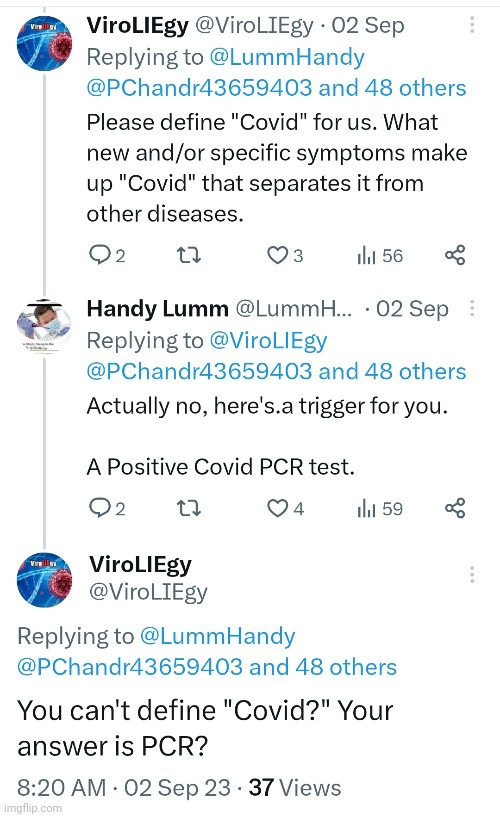
These “tests” were never calibrated and validated to purified and isolated “virus” in order to accurately detect what they are claimed to be detecting. Despite this fact, PCR tests are now commonly used to identify tiny fragments of a theoretical genome that was assembled from RNA of unknown provenance claimed to belong to a “virus” that has never been scientifically proven to cause any disease. This is how a “Covid” case is determined. That is why the below response that I received that the definition of “Covid-19” is a positive PCR result, coming from a person who identifies as an HCPC registered Biomedical Scientist working in the hospital lab, is not as absurd as it first may sound.
“Covid-19” truly is nothing but a positive PCR result. That's it. This is why a “new disease” called “Covid-19” can be found mostly in the asymptomatic, i.e. healthy people, who are not suffering from any disease whatsoever. This is why the symptoms belonging to "Covid” can range from none to the common cold, to Kawasaki disease, to frost bite, and all the way to death. This is why the CDC was able to add six “new” symptoms to “Covid” in April 2020, over four months after the common symptoms of pneumonia were first identified in patients in China, upon the introduction of mass testing. When one is labelled as a “Covid” case based upon a fraudulent test, any symptoms that they may or may not experience as well as any underlying health conditions that they may have had, become absorbed into the “Covid” umbrella. However, this amalgamation of unrelated symptoms joined together by way of PCR does not make “Covid” a new disease. It never was. It is simply the brand name for the positive PCR result, a result that is admittedly inaccurate when disease prevalence, which requires cases to be diagnosed clinically, is low. As “Covid” cannot be diagnosed clinically based upon specific signs and symptoms, there is no way to get an accurate disease prevalence rate in order to determine the accuracy of the PCR result. Thus, PCR is used to generate cases in order to calculate disease prevalence so that its results can be claimed as accurate. However, PCR cannot be used to create cases in order to determine its own accuracy. This is outright fraud, and it is the very reason why there was never any “viral pandemic.” It has always been, and will continue to be, a testing pandemic until enough people become aware of the truth and stop testing for a “new disease” that never existed in the first place.
Here is an excellent article by Steve Falconer, presented by Michael McKay, that examines 32 key questions one should ask themselves as well as their doctors.
provided a straightforward challenge that anyone can utilize to fend of the 🤡 knocks it outta the park again with her latest examining the 5 spectacular fails from germ theor…er, I mean hypothesis. 😉








A. "What does the test do?"
B. "It finds COVID."
A. "And how do we know that it finds COVID?"
B. "Because people with COVID tested positive with this test."
A. "And how do we know they had COVID?"
B. "Because they tested for it."
I have had a lifetime of "strep throats" and "chest colds" and "bronchitis." Every time I had a respiratory tract infection, I lost my sense of smell and taste. I figured that since my head and throat were clogged with mucus, that gunk was blocking my olfactory sensors. So the uber-propaganda of the C-19 daily media flogging, with their loss of smell and taste hysteria, was an immediate red flag to me! It was clear that the MSM "news" was lying every night in Jan, Feb, Mar 2020. I turned it off and was shocked that there many "educated" people I knew believed it!
Other than the 1950s-60s "vaccines," I have never had a "flu" shot, and believed bouts of sickness actually strengthened my immune system. And then I discovered how massively poisoned I was as a teenager by my mother who allowed a dentist to fill 16 molars (that had no cavities) with mercury amalgam fillings, as "preventative dentistry."
The sources of poisons which debilitate humans, animals and plants are massive. Sally Fallon Morrell at the Weston A. Price website, has a couple of dandy articles. One asks if the real cause of anthrax is arsenic poisoning, and the other hypothesizes that tuberculosis could be iron oxide poisoning. I am half-way through "The Invisible Rainbow" by Arthur Firstenberg. These other theories about what makes us sick are very interesting to me ... as it's clear the "virus model" has completely collapsed. Many thanks to the diligent brains behind the "no viruses" model!!