“Group A streptococci (Streptococcus pyogenes) (GAS) are a relatively common infection that is often asymptomatic and when symptomatic most typically causes a sore throat though at times can cause other more serious diseases such as scarlet fever, skin infections, rheumatic fever and rarely streptococcal toxic shock syndrome.”
-Prof Paul Hunter, Professor in Medicine, University of East Anglia (UEA),
There has been a recent surge in scary tales circulating in the mainstream media headlines over a sudden rise in the cases of Strep A. Terrifying stories are making the rounds to frighten parents enough so that they will take their children to be tested for a relatively common symptom.
However, it is reported by the WHO that the Strep A cases and the risk posed to the general public is relatively low:
WHO currently assesses the risk for the general population posed by the reported increase in iGAS infections in some European countries as low, considering the moderate rise in iGAS cases, GAS endemicity, no newly emerging emm gene sequence types identified, and no observed increases in antibiotic resistance.
https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON429
Unfortunately, this has not stopped an overreaction fueled by fear-based media propaganda. The panicked response generated by misleading headlines feeds a sick cycle that generates more cases with increased testing which allows for this fear-based narrative to continue to pick up steam to be reported on by the media to further fuel the panic level. We've seen this in recent years with “covid,” monkeypox, polio, ebola, etc. However, sore throat is amongst the most common symptoms that is experienced on a regular basis, especially during the winter season when the air is particularly dry and affects the throat:
“Pain in the throat is one of the most common symptoms, which accounts for more than 2% of all adult primary care visits each year.
Most sore throats are caused by infections, or by environmental factors like dry air. Although a sore throat can be uncomfortable, it will usually go away on its own.”
https://www.healthline.com/health/sore-throat#What-is-a-sore-throat?
This leads one to wonder, as the cases and risk of infection are admitted to be low and this relatively common symptom can be easily explained by environmental conditions, is the Strep A hype yet more manufactured media frenzy? Without the fear-based propaganda being paraded by the MSM, would parents be rushing their children to get tested for Strep A? Would clinicians even be concerned with performing testing looking for this particular bacteria if they were not on alert to be on the lookout for it? Are the tests even accurate enough to make a diagnosis? Is Strep A found in every case of those who are experiencing this symptom of disease? What about those who are healthy yet pegged with the bacteria despite a lack of any symptoms? Let's explore some of these questions more in depth.
According to the CDC, cases of a sore throat are usually “viral” and will clear up on their own. As long as the patient exhibits symptoms that are considered “viral” in nature, they are not tested for Strep A. It is only when these “viral” symptoms are absent that either the rapid antigen test (with varying sensitivities) is utilized or a throat culture, considered the gold standard test, is performed:
Diagnosis and testing
“History and clinical examination can be used to diagnose viral pharyngitis when clear viral symptoms are present. Viral symptoms include:
Cough
Rhinorrhea
Hoarseness
Oral ulcers
Conjunctivitis
Patients with clear viral symptoms do not need testing for group A strep. However, clinicians cannot use clinical examination to differentiate viral and group A strep pharyngitis in the absence of viral symptoms.
Clinicians need to use either a rapid antigen detection test (RADT) or throat culture to confirm group A strep pharyngitis. RADTs have high specificity for group A strep but varying sensitivities when compared to throat culture. Throat culture is the gold standard diagnostic test.”
https://www.cdc.gov/groupastrep/diseases-hcp/strep-throat.html
The signs and symptoms listed by the CDC that typically distinguish between bacterial versus “viral” cases of a sore throat include a cough, runny nose, hoarseness, and conjunctivitis. This leads one to wonder, as the symptoms are the same between “viral” and bacterial cases minus those common symptoms which are falsely attributed to “viruses,” are these common “viral” symptoms always absent in cases of strep throat? While these symptoms are considered to be less common, they do occur in cases of strep throat thus making the diagnosis based on clinical symptoms alone meaningless:
13 Symptoms That Tell The Difference If It’s Strep Throat
Runny Nose
“When strep throat is the cause of a sore throat the symptoms are typically focused on the throat. This means that the other symptoms such as a runny nose or chest congestion are not as common. A person suffering from strep throat may have a bit of mucus in the throat or a bit of congestion, but strep throat typically does not affect the nasal cavity.”
Hoarseness
“One of the most common effects of strep throat is losing your voice. A person who is suffering from strep throat may find it difficult to speak. When you speak, air passes through the windpipes. This can cause pain in the area of the throat if you are suffering from strep. While a cold or throat irritation may make speaking difficult, with strep the symptom is often more severe.”
Cough
“As mentioned, strep throat is spread through coughing and sneezing. While one of the symptoms of strep throat is a sore throat without a runny nose, strep throat can cause a person to sneeze more than normal. Coughing when you have strep can be quite painful. However, the build-up of mucus in the throat can make it difficult to breathe and you need to clear out your throat.”
https://stayhealthy.fit/13-symptoms-tell-difference-strep-throat/5/
Strep and Eye Infections
Conjunctivitis
“Group A strep can cause an eye infection. Group A also usually causes strep throat and can also lead to more serious infections, such as scarlet fever.
Bacterial conjunctivitis: Conjunctivitis involves an infection of the clear tissue that is over the white part of the eye. It can occur due to a virus or a bacterium. One of the most common causes of bacterial conjunctivitis is streptococci. Symptoms of conjunctivitis include:
Pink eyes
Watery eyes
Gritty feeling in the eyes
Itchiness
Irritation
Burning
As runny nose, cough, hoarseness, and pink eye can be found in cases of sore throats that are considered caused by Strep A, the presence or absence of these symptoms can not be used to make a definitive diagnosis. Regardless of what the CDC wants us to believe, there are no specific symptoms differentiating between a “viral” case and a bacterial case of a sore throat. The only reason the four symptoms listed above are offered as distinguishing criteria is to rule in or out testing for Strep A. When these symptoms are present, the doctor assumes a “viral” cause and sends the patient home without testing or treatment. However, this does not mean that the patient would not have tested positive for the streptococcus bacteria if these “viral” symptoms are present. The bacteria is just assumed not to be the cause.
As the symptoms overlap between sore throats caused by “viruses” and bacteria, the only way to get a positive diagnosis for Strep A is said to be through testing. The inability to differentially diagnose between “viral” and bacterial cases of a sore throat clinically was the main reason behind updated 2002 recommendations made by the Infectious Diseases Society of America which established a reliance on testing to confirm a diagnosis:
Diagnosis of Strep Throat in Adults: Are Clinical Criteria Really Good Enough?
“The clinical manifestations of group A streptococcal and nonstreptococcal pharyngitis overlap quite broadly. For this reason, the updated Infectious Diseases Society of America practice guideline for group A streptococcal pharyngitis, published in this issue of Clinical Infectious Diseases, recommends laboratory confirmation of the clinical diagnosis by means of either throat culture or a rapid antigen detection test.”
https://academic.oup.com/cid/article/35/2/126/396412
The most common testing performed in the past was by way of throat cultures as it is considered to be the gold standard diagnostic tool. However, this method has been phased out in recent years in favor of the rapid antigen (Strep) test in order to quickly diagnose a case. As 70-85% of the cases of sore throats are considered to be “viral” in nature (minus any testing whatsoever), the only reason either the RST or throat culture is used is in the absence of the four symptoms discussed above which “suggest” a “viral” cause.
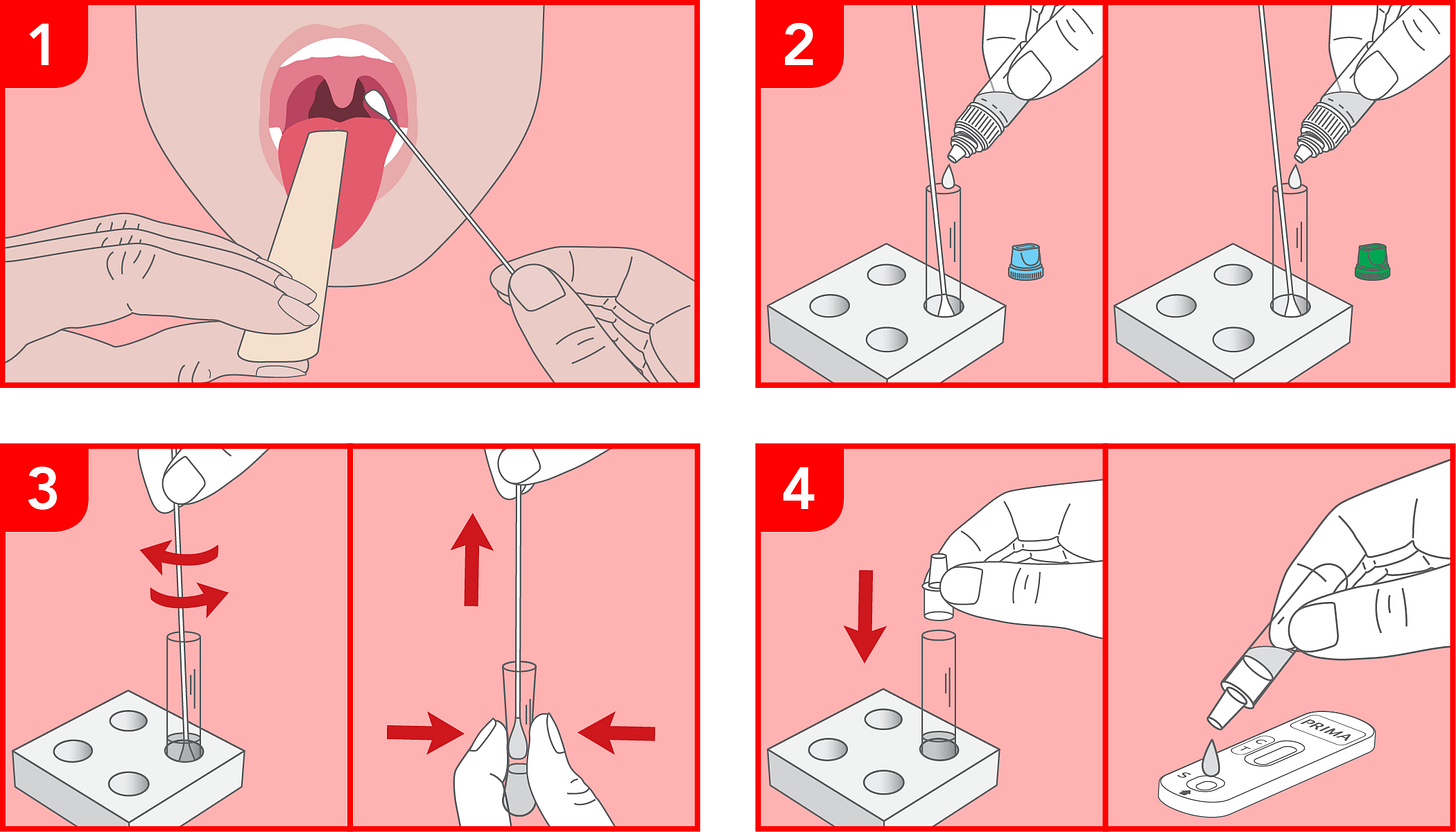
As testing is said to be the only way to definitively distinguish between “viral” and bacterial cases of a sore throat, it would be a good idea to investigate these methods a bit more. To gain some valuable insight into the limitations of the testing methods used in the instances without “viral” symptoms, let's look at a 2018 article which appeared in the Physician’s Office Resource and see what we can uncover. Starting with the rapid strep test (RST), a person's throat is swabbed to collect a sample of mucus. This sample is then mixed with a chemical reagent said to contain antibodies which is added to a test strip that is designed to look for antigens said to be specific to the streptococcus bacteria. If the antigens are present, it is stated that they will migrate along a film to form a visible line of antigen bound to the labeled antibodies. If you know anything about antibodies, this should be a red flag on the accuracy of the results.
According to estimates, the RST tests are said to be highly specific (95%), meaning it produces less false-positives, yet it suffers from lower sensitivity (70-90%) meaning it leads to greater false-negatives. Interestingly, it is stated that some of the rapid strep tests are not waived (i.e. approved) and thus they require proper certification or accreditation before use. The article states that neither throat culture nor RSTs can accurately differentiate acutely infected persons from asymptomatic streptococcal carriers with “viral” pharyngitis. In other words, the results are essentially meaningless. On top of that, living or dead strep bacteria will produce a positive reaction thus the test can not state whether one is infectious nor that the bacteria is the cause of the symptoms of disease. Even though it is claimed that false-positives with RST's are rare, false-positive results are “indicative of similarities between various surface proteins found on strep bacteria and other non-strep bacteria found in the mouth” thus showing that cross-reactions occur in the test with non-strep bacteria. This would mean that these antigens are not specific to streptococcus. This should raise doubt to the validity of any of the results generated through the RST.

Turning our attention to the “gold standard” throat culture test, a swab is inserted into the back of the throat and the sample obtained is used to culture the bacteria on a special plate in a lab. The article points out that, if performed correctly, throat culture is said to be 90%–95% sensitive for detection of GAS pharyngitis. However, there are several variables which can affect the accuracy of this method. These include:
The manner in which the swab is obtained which has an important impact on the yield of streptococci.
Antibiotic use before the swab test is performed leading to false results.
The duration of the culture incubation can result in more positive cases if performed for 48 hours or longer.
The clinical significance of the number of GAS colonies on the throat culture plate is problematic as there is too much overlap between acute vs chronic carriers of the bacteria to permit accurate differentiation on this basis alone.
Thus, it is clear that the accuracy and interpretation of both the RST and the throat culture test could be considered of a questionable nature in determining a meaningful Strep A diagnosis:
Group A Streptococcal Pharyngitis Testing Guidelines & Procedural Limitations
“Strep tests are used to determine if a person with a sore throat (pharyngitis) has strep throat, an infection of the throat and tonsils caused by the bacteria Streptococcus pyogenes, also called Group A Streptococcus (GAS), or if the sore throat is caused by a virus. The majority of sore throats (70%-85%)1 are actually viral in nature, and will resolve without treatment within a few days.”
Establishing the Diagnosis of GAS Pharyngitis6
“1. Swabbing the throat and testing for GAS pharyngitis by rapid strep test and/or throat culture should be performed because clinical features alone do not reliably discriminate between GAS and viral pharyngitis except when overt viral features like runny nose, cough, oral ulceration, and/or hoarseness are present. In children and adolescents, negative rapid strep tests should be backed up by a throat culture; however, positive rapid strep tests do not necessitate a back-up culture because they are highly specific.”
Who Should Undergo Testing for GAS Pharyngitis?7
Testing for GAS pharyngitis usually is not recommended for children or adults with acute pharyngitis with clinical and epidemiological features that strongly suggest a viral basis (e.g, cough, runny nose, hoarseness, and oral ulceration).”
Testing Guidelines
l. The Rapid Strep Test (RST)
Description
A major disadvantage of throat cultures is the delay (overnight or longer) in obtaining results. RSTs have been developed for the identification of GAS pharyngitis directly from throat swabs, with shorter turnaround time. Rapid identification and treatment of patients with GAS pharyngitis can reduce the risk of spread, allowing the patient to return to school or work sooner, and can reduce the acute associated morbidity. The use of RSTs for certain populations (e.g, patients in emergency departments) was reported to significantly increase the number of patients appropriately treated for streptococcal pharyngitis, compared with traditional throat cultures.
RSTs currently available are highly specific (approximately 95%) when compared with blood agar plate cultures. False-positive test results are highly unusual, and therefore therapeutic decisions can be made with confidence on the basis of a positive test result. Unfortunately, the sensitivity of most of these tests is 70%–90%, compared with blood agar plate culture.
The first RSTs used latex agglutination methods, were relatively insensitive, and had unclear end points. Newer tests based on enzyme immunoassay techniques offer increased sensitivity and a more sharply defined end point.
The practitioner should be aware that some of these rapid strep tests are not waived, and therefore, require proper certification or accreditation of the physician's laboratory. Neither conventional throat culture nor RSTs accurately differentiate acutely infected persons from asymptomatic streptococcal carriers with viral pharyngitis. Nevertheless, they allow physicians to withhold antibiotics from the great majority of patients with sore throats for whom results of culture or RST are negative. This is of extreme importance, because nationally up to 70% of patients with sore throats seen in primary care settings receive prescriptions for antimicrobials, while only 20%–30% are likely to have GAS pharyngitis.
Since the sensitivities of the various RSTs are <90% in most studied populations of children and adolescents, and because the proportion of acute pharyngitis due to GAS in children and adolescents is sufficiently high (20%–30%), a negative RADT should be accompanied by a follow-up or back-up throat culture in children and adolescents, while this is not necessary in adults under usual circumstances, as noted above.
Procedure
Obtaining a specimen is the same whether your doctor will do a throat culture or rapid test for strep. A cotton swab (similar to a Q-tip) is quickly rubbed over both tonsils as well as the back wall of the mouth (the posterior pharynx). It is important to avoid contact with other structures inside the mouth such as the tongue or cheeks. The swab is then placed in a specialized container and the rapid test performed. Many people find that obtaining the swab produces a gagging sensation. However, since the entire swabbing process lasts less than five seconds this inconvenience is minimal.
Limitations
There are several manufactures of rapid strep tests. Each manufacturer has designed their test to respond only to the presence of the particular streptococcal bacteria (Group A) responsible for strep throat. Other bacteria which are less much less likely to cause sore throats are not identified by the rapid strep test.
The test will not detect viral causes of sore throat.
A positive test response occurs when a reaction occurs between a protein on the surface of strep bacteria and chemicals in the test materials. Either living or dead strep bacteria will produce a positive reaction. A positive culture requires antibiotics, nevertheless.
Most rapid strep tests have a sensitivity of 90%, meaning that the test will be positive in 90 of 100 patients who are documented to have strep throat via throat culture obtained at the same time. Since 10 of 100 patients with strep throat will be missed using a rapid strep test, all negative swab specimens should be sent for culture to confirm the absence of strep bacteria.
The rapid strep test has a 98% specificity. This means that 98 of 100 positive tests correctly indicate the presence specifically of Group A streptococcus bacteria; 2 of 100 positive results are \"false positives\" - indicative of similarities between various surface proteins found on strep bacteria and other non-strep bacteria found in the mouth.
ll. The Throat Culture
Culture of a throat swab on a sheep-blood agar plate has historically been the standard for the documentation of the presence of GAS pharyngitis in the upper respiratory tract and for the confirmation of the clinical diagnosis of acute streptococcal pharyngitis. If performed correctly, culture of a single throat swab on a blood agar plate is 90%–95% sensitive for detection of GAS pharyngitis. A major disadvantage of throat cultures is the delay (overnight or longer) in obtaining results. This spurred the development and adoption of rapid strep testing directly from throat swabs, with shorter turnaround time11.
Limitations
Several variables affect the accuracy of throat culture results. For example, the manner in which the swab is obtained has an important impact on the yield of streptococci. Throat swab specimens should be obtained from the surface of either tonsils (or tonsillar fossae) and the posterior pharyngeal wall. Other areas of the oral pharynx and mouth are not acceptable sites. Healthcare professionals who try to obtain a throat swab from an uncooperative child without immobilizing the neck may obtain a specimen that is neither adequate nor representative. In addition, false-negative results may be obtained if the patient has received an antibiotic shortly before the throat swab is obtained.
Another variable that can affect the throat culture result is the duration of incubation. Once plated, a culture should be incubated at 35°C–37°C for 18–24 hours before reading. Additional incubation overnight at room temperature may identify a number of additional positive throat culture results. Thus, although initial therapeutic decisions may be made on the basis of overnight culture, it is advisable to reexamine plates at 48 hours that yield negative results at 24 hours.
The clinical significance of the number of GAS colonies on the throat culture plate is problematic. Although patients with true acute GAS pharyngitis are likely to have more strongly positive cultures than patients who are streptococcal carriers (i.e, individuals with chronic GAS colonization of the pharynx), there is too much overlap in this regard to permit accurate differentiation on this basis alone.
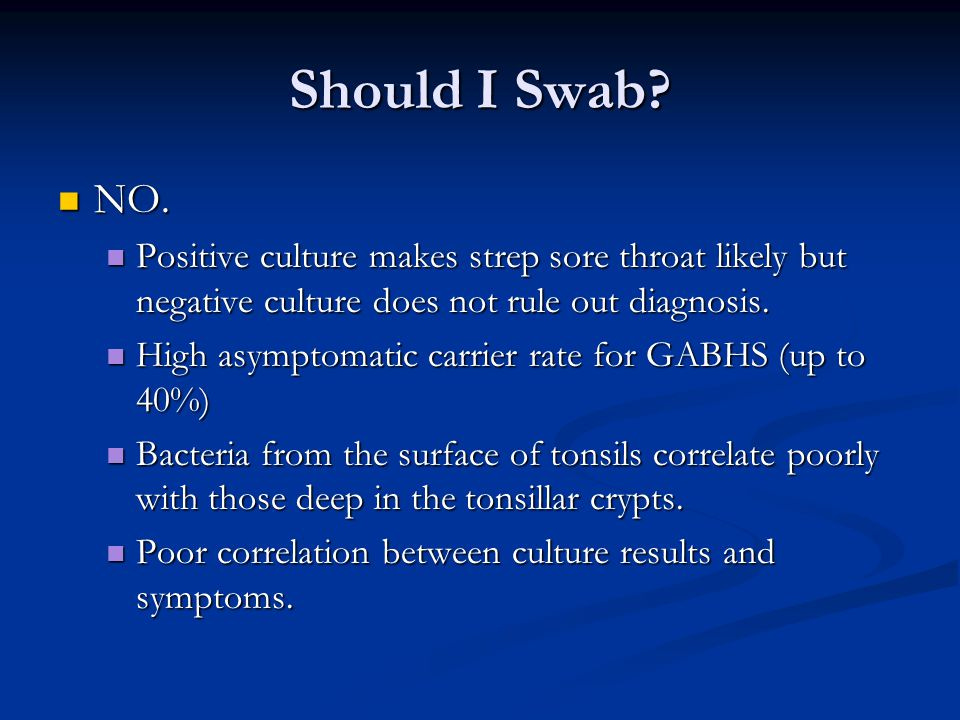
It is clear that the RST's are only able to determine if the bacteria is present but not that it is the cause of disease. The RST's are unable to differentiate between a patient with a true “infection” and one who is a “carrier state.” Remember this as we will discuss the “carrier state” more in a moment. The accuracy of the interpretation of the RST is based upon having a valid gold standard to calibrate and validate against. As stated earlier, the gold standard for Strep A testing is the throat culture. However, as outlined above, the throat culture is also prone to limitations. It too can not differentiate between those who are considered healthy carriers of the bacteria and those who are said to be experiencing disease because of the presence of the streptococcus bacteria. What does it mean for the accuracy of the RST when the results coming from the gold standard itself are uninterpretable?
A study from 1979 critically examined the gold standard throat culture and argued against its use in the diagnosis of Strep A. In this study, it was admitted that diagnosing pharyngitis due to Strep A is extremely difficult, even though it had been over 100 years since the discovery of the bacteria by Louis Pasteur. The authors noted that there are too many limitations of the throat culture method and the interpretation of the results for it to be relied upon in regards to a definitive diagnosis. There were various incriminating reasons provided for this statement such as:
The recovery rate of the bacteria is never 100% and is often much less with only 68% recovery in cases of Scarlett fever.
There are high false-positive rates of up to 40% due to overreading of the results.
Asymptomatic carriers can make up to 40% of the cases which is misleading as “infestation” does not mean “infection” and the bacteria is not always pathogenic.
The bacteria is regularly found as a “secondary infection” in “viral” cases of pharyngitis and is not considered to be of any harm to the individual.
The amount of colonies grown is not an indicator of disease as there can be many colonies or few colonies at any given time in cases of Scarlett fever.
In over half of the cases of acute pharyngitis after full “viral” and bacterial investigation, no etiological agent or cause can be identified.
A positive culture with acute pharyngitis does not mean that there is an active infection and in 57% of cases, it was shown not to be the cause of the symptoms even though the bacteria was present.
There is an old adage that Strep A can not be diagnosed clinically and diagnosis must be reliant upon the throat culture, yet this article shows the errors in relying on the gold standard.
A Case Against the Use of the Throat Culture in the Management of Streptoccocal Pharyngitis
“Although one hundred years have now passed since the discovery of streptococcus pyogenes by Louis Pasteur, in the blood of a patient with puerperal septicemia, the definitive identification of pharyngitis due to this organism is still extremely difficult.
It is suggested here that the throat culture has too many problems associated with its use and interpretation, that it is of little value in supplying concrete bacteriological diagnosis, and that clinical decision making in acute pharyngitis, without a throat culture, is both rational and acceptable.
The Misleadingly Negative Throat Culture
In streptococcal pharyngitis the throat culture may be negative for the streptococcus since recovery rates for the organism are never 100 percent and are often very much less. Scarlet fever is an incontestably streptococcal disease and yet, in a collection of ten studies, the positive throat culture rate was as low as 68 percent. In a group of patients undergoing tonsillectomy, preoperative throat cultures were positive for beta hemolytic streptococcus 16.4 percent of the time, yet culture of the excised surgical tissues had a positive culture rate of 32.7 percent. It would appear that throat swabs can be a poor index of the presence of tonsillar streptococci.”
The Misleadingly Positive Throat Culture
In nonstreptococcal or viral pharyngitis the throat culture may be positive for the streptococcus. This may happen because of overreading the culture plate, the streptococcal carrier state, or by secondary bacterial overgrowth.
Overreading
Several investigators find a high incidence of overreading of office cultures because of confusion between alpha and beta hemolysis, or between the beta hemolytic streptococcus and other beta hemolytic organisms. False positive rates were 40 percent, 36 percent, and 21 percent. Overreading office cultures for false positive results may be as great a problem as false negative cultures.
The Carrier State
The asymptomatic general population always has an incidence of positive throat cultures which varies with the age group and the season of the year from 10 to 40 percent. When a streptococcal carrier acquires a viral respiratory tract infection and sees a physician who takes a throat culture, the diagnosis will be that of a streptococcal illness. Infestation, however, is not the same as infection. The streptococcus, although a potential pathogen, is not always pathogenic. The organism can exist for months in the throats of healthy people, peaceful coexistence between it and its host being the rule and disease the exception. The carrier rate, which is inversely proportional to the streptococcal illness rate, is a valuable asset to the individual, who is not ill, not contagious, and not at risk for rheumatic fever. A carrier will be found to be in the process of acquiring specific M type immunity to his streptococcal strain in a natural way, and because of substrate competition, bacterial interference, and cross protection among the types of group A streptococci, he may well be less likely to acquire a new virulent epidemic strain. The carrier should be left untreated, even when he has a viral pharyngitis.
Secondary Bacterial Overgrowth
There is a synergism between streptococci and viruses in the respiratory tract, the bacteria frequently appearing as secondary invaders in the later course of a viral illness. In smallpox, measles, influenza, and other viral respiratory tract infections, streptococci, often nonepidemic strains of low virulence, invade the throat and grow luxuriantly. Because of this synergism it is understandable that a patient with a viral infection may have a positive throat culture for beta hemolytic streptococcus, even with heavy growth on the culture plate, and not be infected by the organism but merely infested, and in no danger of harm.
Thus, in acute pharyngitis the throat culture may be misleadingly positive because of overreading, the carrier state, or bacterial-viral synergism. The presence of a positive throat culture in a patient with acute pharyngitis does not exclude the diagnosis of viral pharyngitis.
The Degree of Positivity of the Culture
It has been suggested by proponents of the use of the throat culture that the number of colonies of streptococci on the culture plate is a useful indicator of the difference between a carrier and a patient with an active infection, the presence of fewer than ten colonies being considered clinically unimportant.
However, in scarlet fever there may be heavy growth on the culture plate, or there may be none. Of individuals in a population study, having a heavy growth on culture, only 38 percent had a rise in antistreptolysin titer; subjects with strongly positive cultures were no more likely to be ill than those with lightly positive ones. In all types of nonstreptococcal respiratory illness and in concurrent viral infections, high streptococcal colony counts have been found, and low colony counts, far from being clinically unimportant, still produce in one third of patients a significant serologic response.
Therefore it is plain that the degree of growth on the culture plate cannot be of any practical use in clinical decision making.
The Syndrome of Acute Pharyngitis
Acute pharyngitis is the problem which the clinician faces and which he/she must manage on the basis of symptoms and signs, with or without the additional factor of the throat culture. Yet the cause of the illness is often obscure. In one half of patients with acute pharyngitis, after full bacteriological and virological investigation, no etiological agent can be found. In the remainder, one third have positive throat cultures for beta hemolytic streptococcus and one sixth are harboring a virus: influenza and parainfluenza, adenovirus, rhinovirus, enterovirus, coxsackie virus, or herpes simplex virus.
It is the one third of acute pharyngitis patients who do have a positive throat culture for beta hemolytic streptococcus that must now be considered. It is this group of patients who are assumed to have streptococcal pharyngitis by those who rely on the culture. Strangely enough, such an obvious assumption is incorrect.
Acute Pharyngitis with a Positive Culture
It was demonstrated in the discussion on the Misleadingly Positive Throat Culture, that a positive culture in a patient with pharyngitis may not be evidence for an active streptococcal infection. An active infection must be defined as the presence of a positive culture plus a subsequent rise in type-specific antibody. It is the magnitude of this rise in antistreptococcal antibody which relates to the risk for the subsequent development of acute rheumatic fever.
It has been found that in fewer than half (43 percent) of acute pharyngitis patients with positive cultures did serological evidence of acute streptococcal infection develop inhibition of antibody response by antibiotics not being a factor. In a majority of the patients (57 percent), the illness could not be related to the streptococcus present in the throat culture. Such patients were usually convalescent carriers with an already high titer of antibody to the strain that they were carrying in their throats, and who had succumbed to an intercurrent viral illness.
These individuals with acute pharyngitis and a positive culture but no serological response were neither at risk of developing complications nor of transmitting infection, and were not, in fact, suffering from streptococcal pharyngitis. Yet, such patients make up more than half of the group assumed to have streptococcal pharyngitis by those who rely on the culture.
The throat culture, with its false negatives and false positives, and its inability to demonstrate active infection, is a failure in the clinical setting.
It is consideration of the efficacy of the clinical assessment of the patient, with clinical diagnosis of streptococcal and nonstreptococcal illnesses, and then consideration of the reasons why streptococcal pharyngitis should be treated at all, that will show that clinical management without a culture is a valid course of activity.”
Conclusions
“The throat culture can miss or overread the streptococcus, and a positive culture may merely reveal a carrier, or secondary overgrowth in a viral infection. The degree of growth on the culture plate is not helpful and less than half of positive cultures denote an active streptococcal infection.
Conversely, clinical syndromes of streptococcal and of viral illness correlate well with positive and negative cultures. Since it is irrational to act on the basis of a culture report when it conflicts with the clinical picture, the culture can be omitted. The possibility of laboratory error confirms the primacy of clinical judgment.
Whatever the result of a throat culture, it is those patients with the clinical features of streptococcal pharyngitis who need antibiotic therapy both for symptomatic relief and for prevention of suppurative complications.
Rheumatic fever is a disease to be attacked by political, social, or public health measures in high-risk areas, not by adding throat culturing to clinical management in an individual practice which can have negligible impact.
“Streptococcal pharyngitis cannot be diagnosed by clinical methods-there must be a throat culture.”
Can this still be said to be true?”
While the above article makes a very damning argument against the use of the gold standard throat culture for the diagnosis of a Strep A infection, it actually is more damaging to the narrative that the bacteria is ever pathogenic in any case where it is found. Remember the “carrier state” mentioned in the article making up (at least) 40% of the positive cultures? This is what we refer to as asymptomatic carriers (i.e. healthy people) today. The article states that peaceful coexistence of these healthy people and Strep A is the rule, while disease is the exception. Why is this important? According to a recent article about the current crop of Strep A cases making the rounds here in 2022, the highest incidence is in asymptomatic school-going children:
What is group A streptococcal infection?
Group A beta-hemolytic streptococcus (Streptococcus pyogenes) is a Gram-positive, aerotolerant bacterium commonly found in the throat and skin. The bacterium is known to colonize the pharynx of asymptomatic people. The highest incidence has been observed among asymptomatic school-going children, with an infection rate of about 8-12% in developed countries and 15-20% in developing countries.
The fact that there are asymptomatic carriers of the streptococcus bacteria immediately rules it out as the cause of the disease, regardless of the claimed “accuracy” of the tests, as it fails Koch's first Postulate for proving a pathogenic microbe:
The microorganism must be found in abundance in all organisms suffering from the disease, but should not be found in healthy organisms.
However, it is well known that many cases of strep A are asymptomatic:
“In many people, Strep A will cause an asymptomatic infection, but others will have a sore throat, scarlet fever, or in very rare cases the severe invasive Group A Strep disease.”
Thus, this bacteria is regularly found in healthy hosts showing that it has no pathogenic potential. This should lead one to the conclusion that finding the streptococcus bacteria in a sick host does not mean that the bacteria is the cause of the symptoms of disease. Remember, correlation does not equal causation. In fact, in many of the cases, the relationship between the streptococcus bacteria and disease has been shown to be the exact opposite as the bacteria is regularly ruled out as a causative agent in favor of the “viral” diagnosis even if it is present. Thus, we have yet another situation where the presence or absence of non-specific symptoms will lead to the tests which will be used to create cases to associate the bacteria with the symptoms of disease when a causal relationship has never been scientifically proven to begin with. This will continue to drive fear-based headlines that will fill frightened parents with enough dread so that a common symptom which regularly clears up on its own will rush them to have their children tested and placed on toxic antibiotics which were never necessary to begin with. Meanwhile, a positive result does not mean that there was an active “infection” nor that the organism detected was the cause of the symptoms of disease it is associated with. Sound familiar?
Special shout out to fellow Iowan Michael McKay for his amazing essay on the problems with virology. He does an excellent job distinguishing between terrain and germ theory and laying down the logical framework for why the terrain is key. I highly recommend giving it a thorough reading!
https://www.gravitypal.com/NewParadigm
For more on the problem with Koch's lst Postulate, asymptomatic carriers, and “proof” of a bacterial cause of disease, please see this article:
https://viroliegy.com/2022/10/10/kochs-postulates-and-the-great-asymptomatic-escape/
had a great two-piece breakdown of the Strep A madness: did an excellent video on Strep A and "super bugs" as well:








It's surprising to me how much different are my judgments now when I read "lists of symptoms of diseases." Now I always think: that must be the self-cleaning mechanism working properly.
And then I think: how did people got contaminated to have to go through that self-cleansing process, and what can they do to avoid more contamination in the future?
Before, I would only think in finding remedies for "inevitabe" diseases. How wrong I was!
So thorough! I was waiting for the analysis at the end that brought it all home and you did not disappoint. I hope your work is a labor of love, Mike. I sure appreciate it!