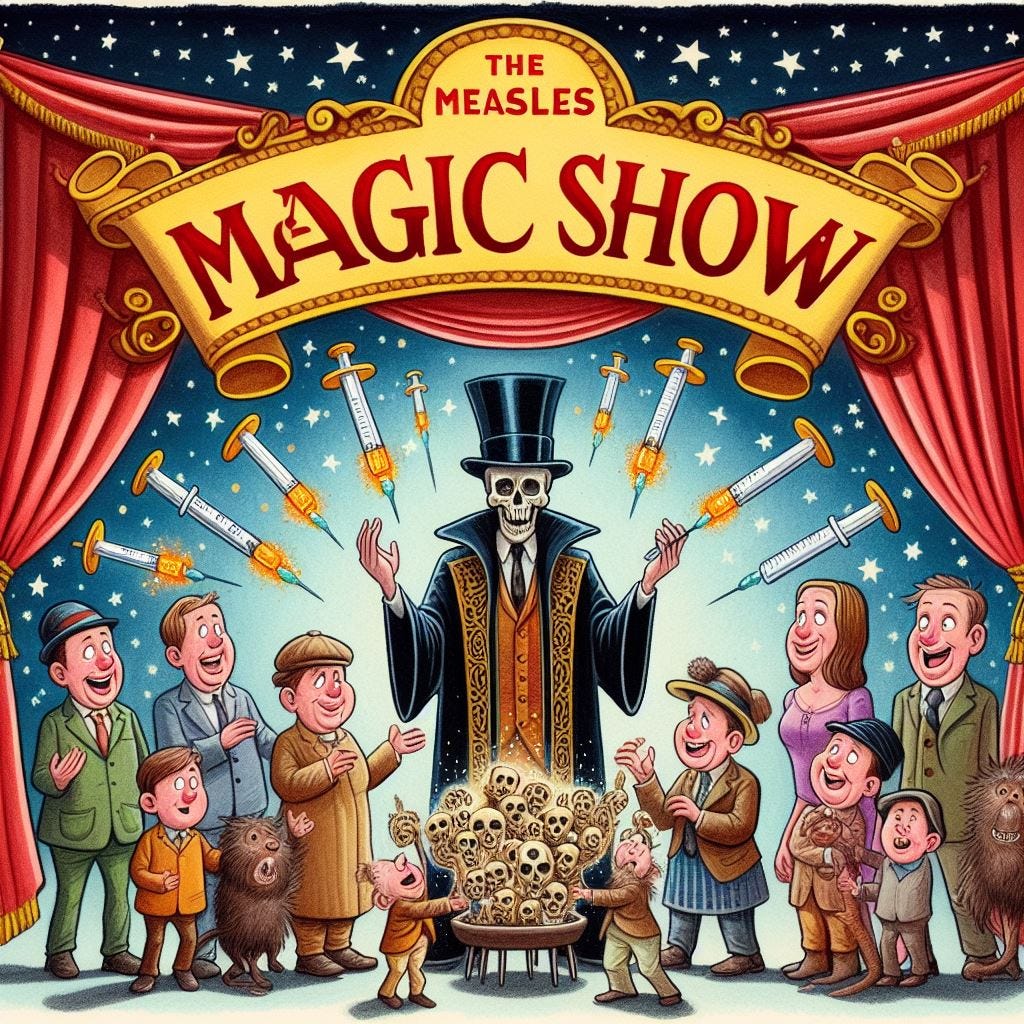
If you have been paying attention to recent headlines here in the US, you will notice that it is time once again for the measles magic show. In other words, it is time for virologists to pull the measles “virus” out of their hats so that it can rear its head in order to frighten the ignorant into allowing toxic injections into themselves and their children. While measles cases are said to occur in the US every year, the alarm bells rung by the CDC and within the mainstream media happens every so often when there needs to be a clamp down on anti-vaccine messaging as well as a push to increase vaccination rates. Remember the scary headlines alerting the people to a measles outbreak in Disneyland in 2014? It was the perfect set-up to strike down nonmedical vaccine exemptions that were increasing in California and elsewhere. The media focused on a “spread” through the unvaccinated population and highlighted vaccine hesitancy as a primary driver of the outbreak. This led to a “positive” outlook and support for vaccination.
Revisiting the 2014-15 Disneyland measles outbreak and its influence on pediatric vaccinations
“The outbreak capped a year with the highest number of measles cases reported in two decades and came amidst increasing trends in nonmedical vaccine exemptions in California and elsewhere. Because of its sensational story line and spread among unvaccinated populations, the outbreak received a high level of media coverage that focused on vaccine hesitancy as a primary driver of the outbreak. This media coverage and the ostensible public support for vaccines that followed led some to hypothesize that the outbreak might have a "Disneyland effect," or a positive influence on the uptake of pediatric measles vaccine.”
https://pubmed.ncbi.nlm.nih.gov/34495822/
However, the Disneyland Measles Massacre wasn't even the “main” measles “outbreak” in 2014. That distinction belongs to the Amish in Ohio where an “outbreak” was blamed on an Amish missionary who traveled to the Philippines. In the end, there were 382 Amish said to be “infected” with the measles “virus.” Not a single person died. Regardless, the missionary, who was originally diagnosed with dengue, was given the blame for being unvaccinated and bringing the measles “virus” back to spread amongst the unvaccinated. While this “outbreak” helped to clamp down on anti-vaccination sentiment riled up by Jenny McCarthy that year, it was the perfect vehicle to convince the masses that it is unvaccinated travelers bringing back diseases in from other countries. This is a theme that the CDC has utilized time and time again:
How an Amish missionary caused 2014's massive measles outbreak
“Last year was terrible for measles in the United States: there were 644 cases — the highest annual caseload in two decades. Granola-crunching Californians, wealthy Oregonians, and Jenny McCarthy anti-vaccine acolytes have taken much of the blame for this spike. The Washington Post even pointed to Orange County — the location of the current Disneyland outbreak — as "Ground Zero in our current epidemic of anti-vaccine hysteria."
But that's wrong. The real story behind the 2014 outbreak isn't on the West Coast. It's in Ohio Amish country, where a missionary returning from the Philippines turned an otherwise unremarkable year for this virus into one of the worst in recent history.”
“The outbreak that Fletcher spent months working to contain ultimately infected 382 Amish Ohioans by the time it was declared over in August of last year. Nobody died, but nine wound up in the hospital with more serious symptoms.”
“But in the first half of 2014 alone, there were 288 cases. And nearly all of them, the CDC researchers wrote in findings published last June, stemmed from Americans traveling abroad and returning with the disease.
"Of the 288 cases, 280 (97 percent) were associated with importations from at least 18 countries," they wrote. Many of these travelers were coming back from the Philippines, which has been dealing with a massive outbreak since fall 2013.
"What we've seen — since the epidemic of measles was interrupted in 2000 — is that we are continually getting measles coming in from overseas," says Jane Seward, deputy director of the viral diseases division at the CDC. "More often than not, it's US residents who go overseas for a trip — to say, Europe, where they don't think they need to be vaccinated. They bring measles back."
“In the Ohio case, "patient zero" had traveled to the Philippines on a missionary trip. (In case you were wondering, he took a plane. Miller explained, "Some Amish fly. Some don't.") At the time, the Philippines happened to be facing a massive measles outbreak, with tens of thousands of cases.
When he returned to Ohio, and fell ill, a doctor misdiagnosed him with Dengue fever, so he continued to pass his disease along to friends and neighbors, many of whom had refused the vaccine out of those concerns over adverse effects.
Fletcher describes it as a "perfect storm:" an unimmunized traveler going to a place with an outbreak and bringing an infectious disease back to an unprotected community.”
https://www.vox.com/2015/1/29/7929791/measles-outbreak-2014
The scare tactics worked to convince some within the notoriously anti-vaccination Amish community to get at least one dose of the MMR vaccine:
Vaccination of Amish limited 2014 Ohio measles outbreak
“In response to the outbreak, which occurred between March 24 and July 23, 2014, some 10,644 members in a community of 32,630 Amish in the Ohio settlement received at least one dose of the MMR vaccine, with 1,585 getting two doses.”
In 2017, there was a growing concern that the Somali community in Minnesota were being influenced by anti-vaccine information. The child vaccination rates for measles, mumps, and rubella (MMR) had plummeted from 92% in 2004 to 42% in 2014 amid fears that Somali children have unusually high rates of autism. Thus, a measles “outbreak” was declared that suspiciously affected primarily unvaccinated Somali children.
“In 2017, 75 measles cases were reported as a result of an outbreak that began in Hennepin County involving the Somali community. This was the largest measles outbreak experienced since 1990, and the second major measles outbreak to affect the Minnesota Somali community in 6 years.”
https://www.health.state.mn.us/diseases/reportable/dcn/sum17/measles.html
Fortunately for the fear promoters, the scare tactics worked again and the vaccination push increased rates amongst the Somali American children from 30 a week in March to 500 in May.
“But the measles outbreak was shifting perceptions at last, she said. Weekly MMR vaccination rates among Somali American children have climbed from 30 or 40 a week in March to about 500 a week in May.”
https://www.bmj.com/content/357/bmj.j2378.long
In 2019, there was a measles “outbreak” in New York City said to have started due to an unvaccinated child who returned home from Israel with measles symptoms. The Orthodox Jewish Community was singled out for their lack of a belief in vaccination as well as their concerns over the dangers of the toxic injections. Thus, a targeted vaccination promotion campaign ensued to combat this growing awareness.
Consequences of Undervaccination — Measles Outbreak, New York City, 2018–2019
“During focus groups conducted by the Department of Health and Mental Hygiene after a mumps outbreak in 2009–201023 in this same community, mothers expressed concern about vaccines and autism, vaccine safety, and whether children are receiving too many vaccines too early in life. Antivaccination sentiments were deepened when an organization targeted this community with misleading materials regarding the risk of vaccination.19 To address these concerns, the Department of Health and Mental Hygiene reprinted and mailed two booklets that provided accurate information about vaccines to 29,000 households in Borough Park and Williamsburg, and a campaign was launched to combat vaccine myths in affected communities.24,25”
https://www.nejm.org/doi/full/10.1056/NEJMoa1912514
The threat of a measles “outbreak” and the vaccination propaganda efforts led to an increase in the percentage of children in Williamsburg who received at least one dose of MMR vaccine, rising from 79.5% to 91.1% among children 12 to 59 months of age. Thus, the scare tactics were once again successful in nudging the sheep in the direction that the pharmaceutical overlords wanted them steered in.
Even though the US officially declared that measles was successfully eliminated (considered an absence of continuous disease transmission for greater than 12 months) from the country in the year 2000, pocket outbreaks tend to conveniently pop up just when there is a growing chorus of anti-vaccination sentiment emerging as well as noticeable decreases in overall vaccination coverage. This is the case now as, due to the declining vaccination rates brought about by the “pandemic” and the distrust in the mRNA vaccines, the “threat” of new measle “outbreaks” in the unvaccinated is being used to try and instill the necessary fear to drive vaccination rates up to where the pharmaceutical interests want them to be. However, with measles eliminated from the US over 20 years ago, how are they able to drum up these measles “outbreaks” right at the most opportune moments in order to propagandize the populace? How are they able to make it look as if the unvaccinated are the main contributors of these “outbreaks?” Let's have a look at a few of the tricks that they have up their sleeves and see if we can take the mysticism out of their magic.
The first part of the trick to increase measles cases is rather easy to spot. The CDC simply sends out an alert to healthcare workers to be on the lookout for any cases of disease that may meet the clinical criteria as a measles case. Prior to any alerts, healthcare workers do not regularly look to measles as a diagnosis if they come across measles-like disease as it is not considered an endemic (a disease that is always present in a population within a geographic area, typically year-round) disease in the US. In the alert, the CDC highlights specific groups who healthcare workers are to be on the lookout for, which is anyone who is linked to international travel as well as anyone who is unvaccinated or partially vaccinated that can be linked to them. However, if a person meets the necessary measles case definition and requirements, but they either had measles in the past or have had their measles vaccines, the CDC assumes that these people are “protected” from the disease and are not measles cases:
CDC warns health care workers to be on alert for measles amid rising number of cases
“The Centers for Disease Control and Prevention (CDC) is warning clinicians to remain on alert for measles cases due to a growing number of infections.
Between Dec. 1, 2023, and Jan. 23, 2024, there have been 23 confirmed cases of measles including seven cases from international travelers and two outbreaks with five or more infections each, according to an email sent this week.”
“According to the CDC, most measles cases in the U.S. occur when unvaccinated or partially vaccinated Americans travel internationally, contract the disease and then spread it to those who are unvaccinated upon their return.”
“The CDC says anybody who either had measles at some point in their life or who has received two doses of the MMR (measles, mumps, rubella) vaccine is protected against measles.”
https://www.yahoo.com/gma/cdc-warns-health-care-workers-220221620.html
From the alert sent out by the CDC, international travel is noted as a condition for suspicion, and it is claimed that most cases are amongst the unvaccinated. Healthcare workers are told to look for anyone presenting with febrile rash and symptoms consistent with measles, which are nonspecific such as cough, coryza, or conjunctivitis. However, it seems that they are to only look to measles as a possible diagnosis if the ill patient traveled abroad, especially to places where measles “outbreaks” are ongoing.
Stay Alert for Measles Cases
“Between December 1, 2023 and January 23, 2024, the Centers for Disease Control and Prevention (CDC) was notified of 23 confirmed U.S. cases of measles, including seven direct importations of measles by international travelers and two outbreaks with more than five cases each. Most of these cases were among children and adolescents who had not received a measles-containing vaccine (MMR or MMRV), even if age eligible.
Due to the recent cases, healthcare providers should be on alert for patients who have: (1) febrile rash illness and symptoms consistent with measles (e.g., cough, coryza, or conjunctivitis), and (2) have recently traveled abroad, especially to countries with ongoing measles outbreaks. Infected people are contagious from 4 days before the rash starts through 4 days afterwards.
Measles cases often originate from unvaccinated or undervaccinated U.S. residents who travel internationally and then transmit the disease to people who are not vaccinated against measles. The increased number of measles importations seen in recent weeks is reflective of a rise in global measles cases and a growing global threat from the disease.”
https://emergency.cdc.gov/newsletters/coca/2024/012524.html
Why does the CDC need to alert healthcare workers to be on the lookout for very specific parameters (such as travel history, vaccination status, certain nonspecific symptoms) in order to look for measles as a potential diagnosis in someone suffering measles-like disease? Shouldn't the healthcare provider be able to look at a measles case and be able to tell what it is in order to diagnose it? If you thought that was the case, you'd be wrong. According to Amesh Adalja, MD, an assistant professor who specializes in “infectious” diseases at the Johns Hopkins Center for Health Security in Baltimore, doctors may suspect measles if there is a history of not being vaccinated that accompanies the nonspecific symptoms of disease, but this suspicion must be “confirmed” with a laboratory test. Even then, some doctors won't suspect measles as they have no idea what a measles case even looks like:
“In general, if a doctor is examining a child with a fever, rash, runny nose and red eyes, and usually some history of not being vaccinated, they will suspect measles,” says Dr. Adalja. A laboratory test that uses a nasal or oral swab can confirm the diagnosis, he adds.
The diagnosis may not always be as straightforward as it sounds, says Adalja. “In the United States, many doctors have never seen a case of measles, and so sometimes they don’t even think to suspect it,” he says.”
https://www.everydayhealth.com/measles/guide/
Dr. Adalja's statement that most healthcare workers have never seen measles and that laboratory confirmation is required in order to make a diagnosis is backed up by the Minnesota Department of Health which stated the same:
“Many U.S. health care providers have never seen a case of measles. Without proper laboratory testing, measles cannot be diagnosed.”
The MN Department of Health reiterated that a clinical diagnosis must be confirmed with laboratory testing in another document as well, meaning that clinical diagnosis alone is unreliable:
"A clinical diagnosis of suspect measles must be confirmed with laboratory testing."
The Washington State Department of Health agreed, saying that clinical diagnosis is unreliable and must be laboratory confirmed:
"Clinical diagnosis is unreliable, therefore cases must be laboratory confirmed."
The National Institute for Health and Care Excellence in the UK also agreed by stating clinical diagnosis is unreliable and must be “confirmed” via laboratory results:
"Measles is a notifiable disease. Clinical diagnosis alone is unreliable, infection must be confirmed by laboratory investigation"
This is further supported in a 2006 paper about measles in the United Kingdom, where it is admitted that doctors do not look for or may not even recognize what to look for with a measles case. Clinical diagnosis is unreliable and laboratory testing is required. Numerous other “causes” of the same fever and maculopapular rash are given such as rubella, parvovirus B19, enterovirus, scarlet fever, human herpesvirus 6, human herpesvirus 7, Kawasaki's disease, meningococcemia, toxic shock syndrome, dengue, HIV, secondary syphilis, and drug eruptions.
Measles in the United Kingdom: can we eradicate it by 2010?
"As clinical experience of measles has declined, doctors in the United Kingdom may not consider the diagnosis nor recognise a case."
"Clinical diagnosis of measles has a low positive predictive value in settings such as the United Kingdom where the incidence is low.23 w15 Laboratory testing is required to confirm the diagnosis and to guide public health management (box 4).23 w15"
"Other causes of fever and maculopapular rash include rubella, parvovirus B19, enterovirus, scarlet fever, human herpesvirus 6, human herpesvirus 7, Kawasaki's disease, meningococcaemia, toxic shock syndrome, dengue, HIV, secondary syphilis, and drug eruptions."
"Every suspected case of measles should be notified. Clinical diagnosis is not reliable and it is therefore essential to return the oral fluid sample for laboratory confirmation"
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1626346/
The reason why the CDC must alert healthcare workers when and how to look for measles cases is because healthcare workers do not actively look for measles cases nor would they know what one looks like if one walked into the office. Plus, just as the CDC assumes that those who are vaccinated are “protected” and cannot possibly have measles, the physicians assume the same as well. This is called evidence of presumptive “immunity.” All that one needs in order to be presumed “immune” to measles, according to the CDC, is one of the following: documentation of vaccination, laboratory evidence of “immunity,” laboratory “confirmation” of measles, or being born before 1957:
Evidence of immunity
"Acceptable presumptive evidence of immunity against measles includes at least one of the following:
written documentation of adequate vaccination:
one or more doses of a measles-containing vaccine administered on or after the first birthday for preschool-age children and adults not at high risk
two doses of measles-containing vaccine for school-age children and adults at high risk, including college students, healthcare personnel, and international travelers
laboratory evidence of immunity*
laboratory confirmation of measles
birth before 1957
Healthcare providers and health departments should not accept verbal reports of vaccination without written documentation as presumptive evidence of immunity."
https://www.cdc.gov/measles/hcp/index.html
We can see that this “presumptive immunity” trick pretty much negates anyone vaccinated as being a “true” measles case or of even being suspected of having the disease even if they match the clinical case definition. According to Chapter 7 of the CDC's Manual for the Surveillance of Vaccine-Preventable Diseases, the definition of a measles case that clinicians are supposed to follow is of an acute illness with a generalized maculopapular rash lasting greater than or equal to three days and a temperature of greater than or equal to 101°F along with cough, coryza, or conjunctivitis. However, in the fine print, the CDC states that the temperature does not need to reach 101°F and that the rash does not need to last equal to or greater than three days in order to “confirm” a measles case, thus making those clinical descriptors essentially meaningless. Also, in the case that someone tests positive for measles via “virus isolation,” PCR, or serology tests, if they have been vaccinated with MMR within 6 to 45 days, they are not considered a measles case.
Case definition for case classification
Clinical description:
An acute illness characterized by:
generalized, maculopapular rash lasting ≥3 days; and
temperature ≥101°F or 38.3°C; and
cough, coryza, or conjunctivitis
Probable:
In the absence of a more likely diagnosis, an illness that meets the clinical description with:
no epidemiologic linkage to a laboratory-confirmed measles case; and
noncontributory or no measles laboratory testing.
Confirmed:
An acute febrile rash illness† with:
isolation of measles virus‡ from a clinical specimen; or
detection of measles virus-specific nucleic acid‡ from a clinical specimen using polymerase chain reaction; or
IgG seroconversion‡ or a significant rise in measles immunoglobulin G antibody‡ using any evaluated and validated method; or
a positive serologic test for measles immunoglobulin M antibody‡§; or
direct epidemiologic linkage to a case confirmed by one of the methods above.
† Temperature does not need to reach ≥101°F/38.3°C and rash does not need to last ≥3 days.
‡ Not explained by MMR vaccination during the previous 6–45 days.
§ Not otherwise ruled out by other confirmatory testing or more specific measles testing in a public health laboratory.
As can be seen in the last highlight in the above fine print, a positive IgM serology test for measles must have not been ruled out by other confirmatory testing for different diseases first. This is due to the issue of a high rate of false positives as measles is not considered “endemic” in the US. Thus, as the risk of false positives are high, the laboratory testing for measles cases is supposed to be restricted to patients “most likely to have measles” which, according to the CDC, includes those who are unvaccinated, those who have a recent history of travel abroad, and those whose symptoms could not be determined with an alternate explanation. In other words, a measles diagnosis is seen as a last resort for a select few candidates, marking yet another trick utilized by the CDC to keep measles cases down and restricted primarily to the unvaccinated population. Interestingly, the CDC admits that many cases of febrile illness and rash may be reported as measles even when they are not “true” cases of measles. They even admit that some vaccinated individuals may be included in with the suspected cases. Thus, they state that laboratory testing must be done to confirm all suspected cases. However, the CDC then states that measles is difficult to “confirm” via laboratory testing in vaccinated individuals.
Because measles is a rare disease in the United States, even with the excellent laboratory tests available, false positive results for measles IgM will occur. To minimize the problem of false positive laboratory results, it is important to restrict case investigation and laboratory tests to patients most likely to have measles (i.e., those who meet the clinical case definition, especially if they have risk factors for measles, such as being unvaccinated, recent history of travel abroad, without an alternate explanation for symptoms, for example epi-linked to known parvovirus case) or those with fever and generalized maculopapular rash with strong suspicion of measles.
During a measles investigation when community awareness is increased, many cases of febrile rash illness may be reported as suspected measles, and the magnitude of the situation may be exaggerated if these cases are included in the absence of laboratory confirmation. This is particularly important as the investigation is ending; at that point, laboratory confirmation should be sought for all suspected cases. Occasionally, suspected cases may include vaccinated individuals. For these cases, laboratory confirmation may be challenging. An overview of diagnostic tools is described below.”
The laboratory tests meant to “confirm” a measles diagnosis include “viral isolation,” PCR, and IgM serology testing. However, negative results in both “viral isolation” and PCR are said not to rule out a measles case as the timing and collection of the specimen affect the results:
"Isolation of measles virus in cell culture or detection of measles RNA by RT-PCR in clinical specimens confirms the diagnosis of measles.
However, a negative virus isolation or negative RT-PCR results do not rule out measles because both methods are affected by the timing of specimen collection and the quality and handling of the clinical specimens."
While they admit to false negative results, the CDC fails to mention that the method used for “virus isolation” refuted itself with the measles “virus” in 1954 and it was shown to be an invalid pseudoscientific experiment. In fact, the results of any cell culture experiment are false results that do not equal “viral isolation.” On top of that, PCR results are admittedly meaningless when a disease is not endemic as in the case of the measles due to the fact that, according to their own sources, a low disease prevalence rate generates high false positive results with PCR. This is a part of the prevalence problem for PCR that nullifies the results.
Regarding serology tests, the CDC states that no single serology test can confirm with 100% confidence every “true” measles case. False positive results are common in those with measles-like disease as well as false negative results in those previously vaccinated. Recently vaccinated individuals may come down with a measles-like disease which means that an IgM serology test cannot be relied upon for some strange reason in order to diagnose whether or not it is measles. The only way for a recently vaccinated person to become a “confirmed” measles case when they experience measles-like disease is to meet the clinical case definition and also be linked to someone else who was a laboratory “confirmed” measles case.
"There is no single serologic laboratory test capable of confirming with 100% confidence every true case of measles."
"Testing for measles-specific IgM from persons with rash and fever can produce false positive IgM results. As discussed above, false negative results can also occur in a previously vaccinated person."
"The occurrence of measles-like illness in recently vaccinated persons can pose particular difficulties. Fever and rash are known to occur 6–12 days post-vaccination in a small percent of vaccinated persons.[1] A positive measles IgM test cannot be used to confirm the diagnosis of measles in persons with measles-like illness who received measles vaccine 6–45 days before onset of rash due to the measles IgM antibody response to the vaccine. Specimens for viral isolation should be obtained in addition to serologic testing (see “Laboratory Testing” section above); isolation of wild type measles virus would allow confirmation of the case. In the absence of strain typing to confirm wild type infection, cases in persons with measles-like illness who received measles vaccine 6–45 days before onset of rash should be classified as confirmed cases only if a) they meet the clinical case definition and b) they are epidemiologically linked to a laboratory-confirmed case."
The CDC admits that it is difficult to diagnose any vaccinated person with measles due to the unreliability of the tests. Perhaps this is why most vaccinated individuals are presumed “immune” to measles and testing is saved for the unvaccinated? Regardless, the CDC acknowledges that even if a measles case is seen at a physician’s office, it is most likely not a “true” measles case even if it meets the clinical definition. The only reason to suspect measles is if the person is unvaccinated and came into contact with traveler's from abroad. Granted, the CDC does say that cases of “high suspicion” should be investigated. However, this is only if other causes have been ruled out first, such as parvovirus, dengue, Kawasaki disease, scarlet fever, and rubella.
“In the measles post-elimination era, most cases of febrile rash illness seen in physician’s offices that meet the clinical case definition will not be measles. However, health care providers should maintain a high index of suspicion for measles in clinically compatible cases especially among unvaccinated persons and among persons who recently traveled abroad or who have had contact with persons such as travelers or international visitors. In addition, not every sporadic measles case is linked to a known importation, so cases that raise high suspicion of measles, irrespective of associated risk factors, should be investigated for measles unless an alternative diagnosis is likely (e.g., known epidemiological link to a parvovirus case).
It is important to consider measles in the differential diagnoses of parvovirus, dengue, Kawasaki disease, and scarlet fever. In addition, when evaluating patients with suspected measles who have negative tests for acute measles infection, additional testing for rubella can be considered."
The list of potential diagnoses for the same symptoms of disease is much longer than what the CDC provided. Going back to the MN Department of Health, a more comprehensive list of diseases, both “infectious” and “non-infectious,” presenting with measles-like symptoms is outlined. As these diseases all have similar features to measles, they all must be ruled out before a measles diagnosis can be made and “confirmed:”
“Providers should also consider other infectious and non-infectious etiologies that may cause fever and generalized rash, including:
Rubella, Scarlet fever, Roseola infantum, Kawasaki disease, Erythema infectiosum (Fifth Disease), Coxsackievirus, Echovirus, Epstein-Barr virus, HIV, Pharyngoconjunctival fever, Influenza
Dengue, Rocky Mountain spotted fever, Zika virus
Dermatologic manifestations of Viral hemorrhagic fevers
Toxic Shock Syndrome, cutaneous syphilis
Drug reactions (e.g., antibiotics, contact dermatitis)
As can be seen from the above information, we are left with quite a few preconditions that must be satisfied in order for a new measles outbreak to be declared.
The CDC must issue an alert for healthcare workers to start looking for measles cases.
Testing should be limited to those who meet the case definition and are unvaccinated, have a recent history of travel abroad, and are without an alternate explanation for symptoms.
Those with a history of previous measles “infection” or vaccination should be presumed to be “immune.”
Many clinicians do not know what a measles case looks like, so clinical diagnosis is unreliable, and it must be “confirmed” via unreliable tests.
The long list of similar diseases presenting with the same symptoms must be ruled out via differential diagnosis first before “confirming” a measles case.
A suspected measles case in someone vaccinated must meet the clinical case definition and be linked to a laboratory case in order to be a “confirmed” case.
With these preconditions firmly established, it is easy to see how the CDC can manufacture and steer a measles outbreak so that it appears as if it was instigated from outside of the US and spread through the unvaccinated. All they need is to alert clinicians in order to have them identify anyone unvaccinated who presents with nonspecific symptoms, such as a fever and a rash, that may have recently been a traveler or been in contact with one. They can then use unreliable laboratory tests to “confirm” that the case is measles rather than any of the other identical conditions it would have been pegged as prior to the alert. If someone who is vaccinated slips through as a suspected case, they make it difficult to confirm them as a measles case by blaming the unreliable tests and the vaccinated status and/or the presumed “immunity.” Thus, a measles outbreak can be steered away from the vaccinated and pinned on any unvaccinated individual when they would have normally been diagnosed with any of the other conditions presenting with a fever, a maculopapular rash, and nonspecific symptoms of disease. Voila! The CDC gets to declare a measles “outbreak” in the unvaccinated instigated from contact coming outside from an “endemic” country. Now that the curtain has pulled back, and the trick has been exposed, it is time to cancel this magic show once and for all.
has two excellent additions this week looking at both syphilis and “rotavirus.” has a slew of new Freedom of Information requests. has a series of pieces on the vitamin fraud. provided a research summary debunking “SARS-COV-2” and “Covid-19.”









I have a paper on the 2011 "measles outbreak" in Quebec, Canada, amongst a 99% vaxxed population. They still blamed the unvaxxed for the incident. I'll link it later.
This sounds like a crime to me. It's called Fraud. But will these con men ever be brought to the bar of justice? I doubt it.
THE CHICKEN OR THE EGG. The Germ Theory Opposed in Song. https://turfseer.substack.com/p/the-chicken-or-the-egg